Tackling Antimicrobial Resistance and MDROs: Leveraging Quality Improvement Tools for Evidence-Based Interventions and Ratios
Read the Magazine in PDF
Abstract :
This report focuses on implementing antimicrobial stewardship measures at Rajasthan Hospital to address the rising incidence of antimicrobial resistance and multidrug-resistant organisms (MDROs). The hospital recognized the need to optimize antimicrobial use, improve patient outcomes, and reduce healthcare costs. The study period covered July 2022 to December 2022, during which data was collected through medication charts, AMS sheets, and direct observations. The findings revealed challenges in knowledge and awareness among healthcare professionals, inconsistent implementation of AMS practices, and issues related to antimicrobial use in clinical practice. To address these issues, educational initiatives, feedback mechanisms, restrictive measures, structural improvements, and policy development were recommended. The results showed significant improvements in clinical outcomes, increased knowledge among staff, effective AMS surveillance, awareness among consultants, reduced morbidity and mortality rates, shortened hospital stays, and enhanced patient satisfaction.
Organizational Profile:
Rajasthan Hospital, a leading multispecialty facility in Jaipur, is driven by the vision of providing healing for all. With modern infrastructure and top-notch amenities, we prioritize creating a healing home rather than just a hospital. Our commitment to excellence is evident in our cutting-edge technology, infrastructure, and clinical care, resulting in improved patient outcomes. Located in the heart of Jaipur, we offer access to renowned doctors and high-quality healthcare at affordable prices. As a NABH, NABL, and ACE-certified hospital, we maintain international standards and provide comprehensive clinical, medical, surgical, and diagnostic services. Our mission is to deliver quality care at an affordable cost, guided by our values of care, transparency, respect, understanding, skill, and teamwork. We are proud recipients of the Best Green Hospital AHPI 2021-22 award.
Introduction:
Rajasthan Hospital initiated an Antimicrobial Stewardship Program (ASP) to improve patient care by ensuring the appropriate and effective use of antimicrobials for inpatients. The program’s objectives included reducing the incidence of resistance, preventing the development of multidrug-resistant organisms (MDROs), minimizing hospital length of stay, and reducing healthcare costs. Top management played a crucial role by allocating necessary resources and fostering collaboration among critical care, pharmacy, infection control, microbiology, doctors, and IT departments. Infection control and active surveillance for Antimicrobial Stewardship (AMS) were prioritised, with a dedicated budget allocated. The hospital also actively participated in the national project PARIVARTAN, further contributing to its commitment to combating antimicrobial resistance as follows:
- The hospital observed an increase in the antimicrobial resistance pattern due to the irrational use of antimicrobials.
- This increase was evidenced in the antibiogram, which reflects the resistance of microorganisms to different antibiotics.
- The incidence of multidrug-resistant organisms (MDROs) also showed an upward trend.
- The study was conducted prospectively, collecting data from medication charts, AMS (Antimicrobial Stewardship) sheets, and direct observations.
- The study period covered from July 1, 2022, to December 2022.
- An AMS audit tool was utilized to evaluate antimicrobial usage and stewardship practices For 100 patients.
In the context of Antimicrobial Stewardship (AMS), several challenges exist within the hospital. Healthcare professionals lack sufficient knowledge and awareness of AMS principles and practices. Additionally, the absence of a functioning AMS committee hinders the coordination and oversight of AMS activities. Although some AMS practices have been introduced, their implementation remains inconsistent and incomplete throughout the hospital. Moreover, there is a prevailing negative attitude towards AMS among healthcare professionals, which can impede the effective implementation and adherence to AMS guidelines. The clinical pharmacy team requires additional staffing, particularly an extra clinical pharmacist, to support AMS efforts. Furthermore, physicians and other doctors have limited involvement and engagement in AMS activities, leading to suboptimal implementation and compliance. The low attendance and participation of healthcare professionals in AMS training sessions further contribute to their limited knowledge and understanding of AMS principles.
Methods:
Despite the availability of Standard Operating Procedures (SOPs) such as the Antibiogram and Antibiotic Policy, their implementation in clinical practice is lacking. Healthcare professionals are not effectively utilizing these SOPs to guide their antimicrobial prescribing decisions. Additionally, there is a noticeable absence of specific forms for collecting data on antimicrobial use and justifying their necessity. This lack of structured documentation hampers the accurate tracking and evaluation of antimicrobial utilization within the hospital. Without proper data collection and justification processes, monitoring trends, assessing appropriateness, and identifying areas for improvement in antimicrobial prescribing practices become challenging.
Process:
Several issues related to antimicrobial use in clinical practice have been identified. These include incorrect dosing, inadequate duration, improper frequency, inappropriate routes of administration, and non-adherence to guidelines for antimicrobial selection.
Delayed initiation, partial compliance with culture- based changes, and inadequate de-escalation are also observed. Medication contraindications and insufficient adherence to surgical prophylaxis guidelines are evident. Moreover, systematic tracking, monitoring, and communication with consultants regarding antimicrobial consumption are lacking.
To find the following, the methods implied were:
- Education – Educational measures can be implemented to address the lack of knowledge and awareness. This includes organizing educational meetings and discussions with coordinators and stakeholders to convey the objectives and goals of Antimicrobial Stewardship (AMS) and Infection Prevention and Control (IPC). An AMS team should be established, educational materials such as clinical practice guidelines for AMS and IPC practices should be distributed, and training should be provided. Reminders can be given verbally or electronically. Additionally, surgical prophylaxis guidelines should be adapted to local needs and effectively disseminated through posters in the operating room.
- Feedback – Feedback plays a crucial role in improving antimicrobial prescribing practices. Regular audits with feedback to prescribers on their prescribing practices should be conducted. AMS should be integrated into ward rounds, patient handover meetings, and local consensus processes for antibiotic treatment or surgical prophylaxis changes. A real-time assessment of prescribed antibiotics should be conducted, providing instant feedback to the prescriber. Redundant therapy should be reviewed, and unnecessary or undesirable treatment should be identified. Dose optimization should also be addressed, considering infection, patient characteristics, antibiotics, and guidelines.
- Restrictive – A restrictive approach can be adopted by restricting formulary drugs and reserving antibiotics for specific cases or situations where their use is warranted.
- Structural – Structural measures involve planning and implementing systems and committees to support IPC and AMS. This includes providing Health Information System (HIS) support for IPC and AMS and having an in-house microbiology department. Setting up a Healthcare Infection Control (HIC) working core committee and an implementation committee can help ensure the proper implementation of AMS and correct IPC practices.
- Policies – Developing and implementing specific policies is essential. This includes setting an antibiotic policy reviewed annually based on the antibiogram. A surgical prophylaxis policy should also be established. Additionally, calculations of defined daily doses (DDD) from the pharmacy can provide valuable insights and support decision-making regarding antibiotic use and monitoring.
Several steps are then taken to secure and replicate the improvement:
For securing the Improvement:
- Leadership commitment
- Establishment of an AMS team
- 6-monthly review of the Antibiogram Daily/weekly review of patient AMS forms by a Microbiologist
- Implementation of AMS key performance indicators, including dose optimization, antibiotic review, escalation and de-escalation rates, MRDO rate, IV to oral switch, and switch of one
- Monthly review meetings
- AMS education through CAHO (Consortium of Accredited Healthcare Organizations)
For replicating the Improvement:
- Leadership commitment
- Establishment of an AMS Committee
- Active participation of senior doctors, especially in critical areas
- Development of a well-structured Antibiotic Policy in consensus with all clinicians
- Active surveillance by clinical pharmacists
- Implementation of a dynamic feedback system
- Training for all healthcare professionals, including consultants, residents, and staff
- Daily monitoring and discussions to ensure adherence to AMS practices.
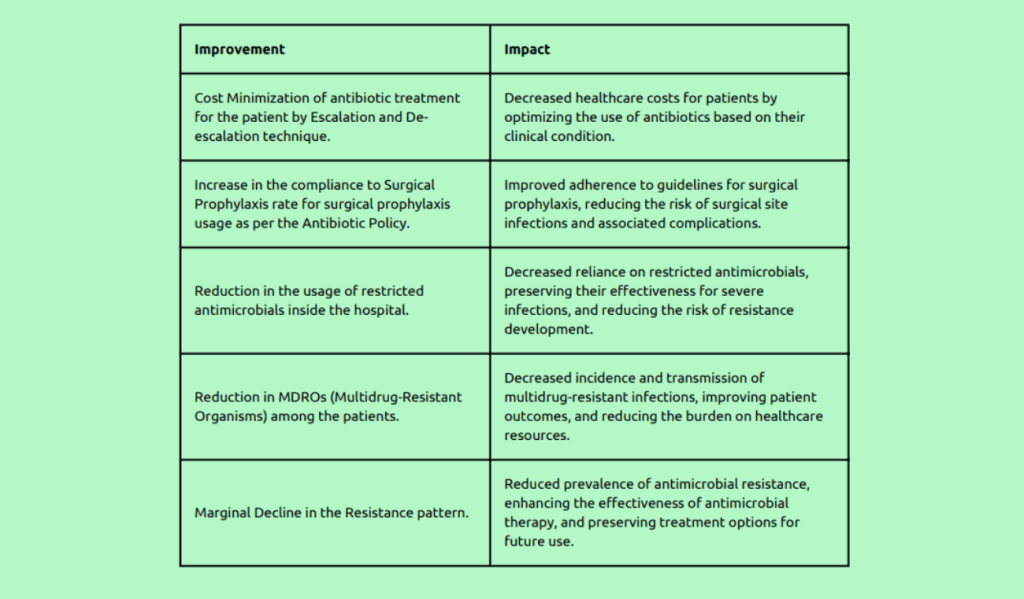
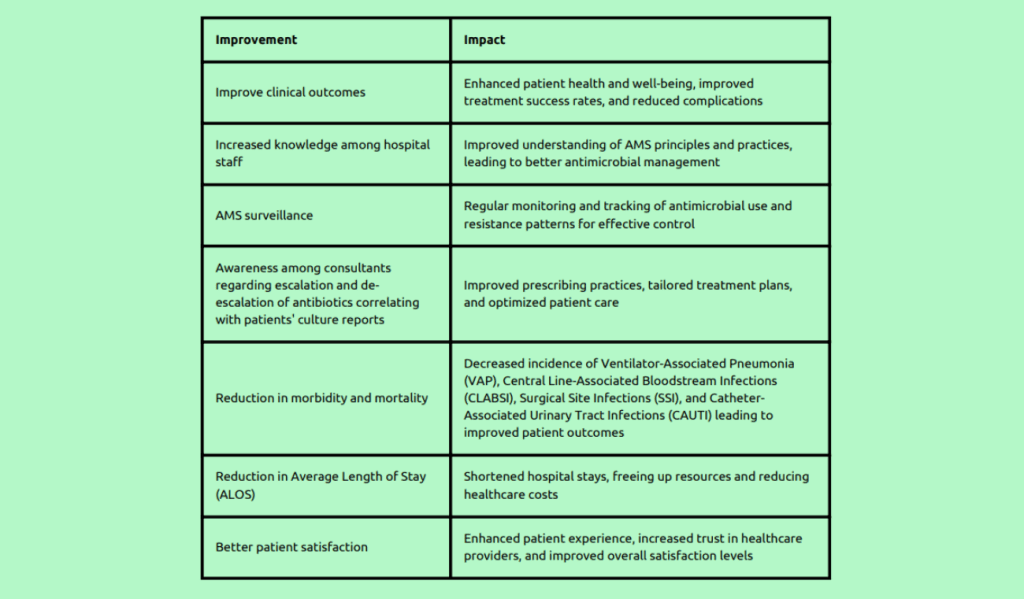
Outcome:
Conclusion
Implementing antimicrobial stewardship measures at Rajasthan Hospital has proven effective in improving patient care and addressing the challenges of antimicrobial resistance and MDROs. By focusing on education, feedback, restriction, structural improvements, and policy development, the hospital has achieved positive clinical outcomes, staff knowledge, surveillance, consultant awareness, morbidity and mortality reduction, length of stay reduction, and patient satisfaction. These findings highlight the importance of a comprehensive and multidimensional approach to antimicrobial stewardship in healthcare settings. Continued commitment, collaboration, and adherence to AMS practices will be essential in sustaining these improvements and further combating antimicrobial resistance.