Teamwork in Healthcare- TeamSTEPPS
Read the Magazine in PDF
Abstract
The article discusses TeamStepps’ implementation (which began in operating rooms) to enhance teamwork and patient safety. TeamStepps addresses barriers to team performance based on four transferable skills: communication, team leadership, situation monitoring, and mutual support. Effective communication and patient involvement as part of the healthcare team are emphasized. Situation monitoring and mutual support are also vital, supported by tools and strategies from TeamSTEPPS. Studies show positive impacts on patient safety culture with its implementation.
Introduction
The Federation of Hospitals implemented the WHO safety checklist in operating rooms to enhance teamwork. However, they felt the need for a method to improve teamwork further and found TeamSTEPPS to be transferable and manageable. TeamSTEPPS is part of the US patient safety movement, aiming to address barriers to team performance that can harm patients.
The training involved one-day sessions and coaches to guide implementation. TeamSTEPPS helps identify and address issues like inconsistent team membership, lack of information sharing, conflicts, fatigue, workload, and distractions. By providing tools to overcome these barriers, TeamSTEPPS enhances teamwork and patient safety. It was initiated in pilot projects in 2005 and publicly released in 2006, while promotion in Switzerland began in 2015 in the Vaud Federation of Hospitals’ Environment.
The TeamSTEPPS model is based on a circle representing the team, with one chapter focused on team composition and structure.
The Federation of Hospitals implemented the WHO safety checklist in operating rooms to enhance teamwork. However, they felt the need for a method to improve teamwork further and found TeamSTEPPS to be transferable and manageable. TeamSTEPPS is part of the US patient safety movement, aiming to address barriers to team performance that can harm patients.
The training involved one-day sessions and coaches to guide implementation. TeamSTEPPS helps identify and address issues like inconsistent team membership, lack of information sharing, conflicts, fatigue, workload, and distractions. By providing tools to overcome these barriers, TeamSTEPPS enhances teamwork and patient safety. It was initiated in pilot projects in 2005 and publicly released in 2006, while promotion in Switzerland began in 2015 in the Vaud Federation of Hospitals’ Environment.
The TeamSTEPPS model is based on a circle representing the team, with one chapter focused on team composition and structure.
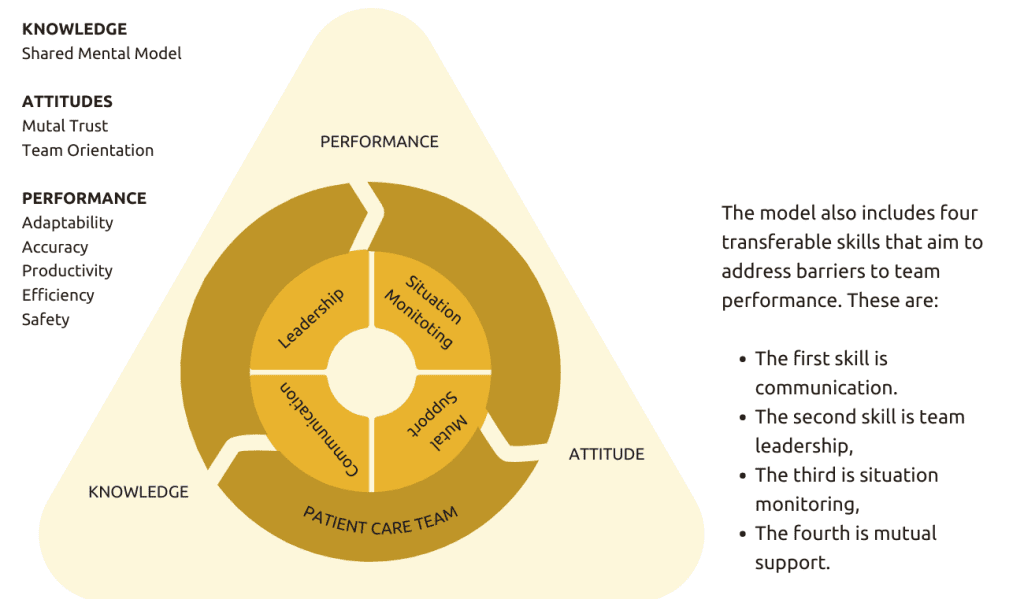
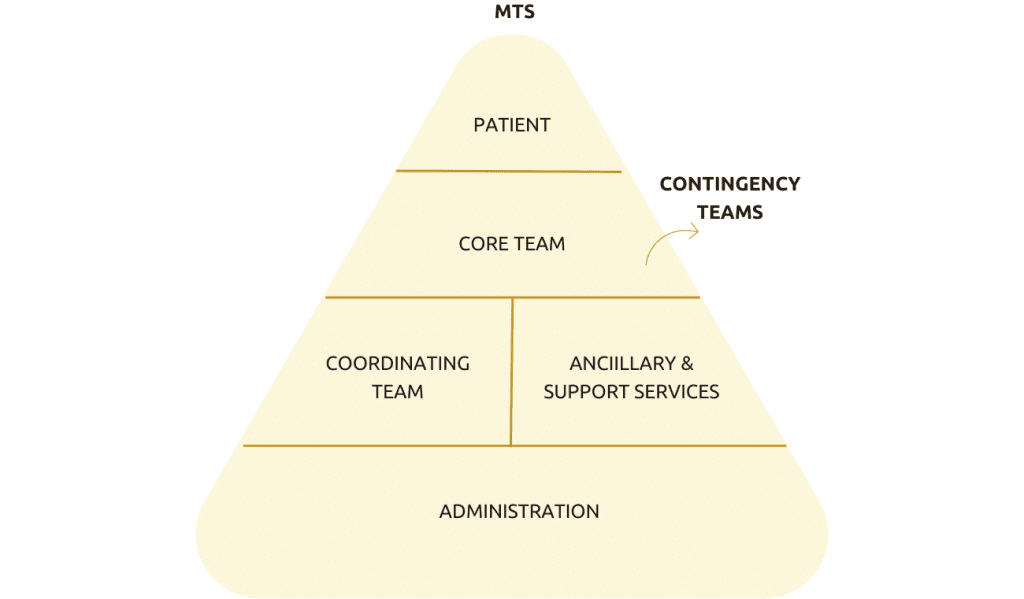
Consistently applying the four TeamSTEPPS skills leads to improved knowledge, attitudes, and performance. This includes increased adaptability, accurate information sharing, efficiency, and safety, ultimately improving patient safety. In the healthcare setting, multiple teams, including the core team at the bedside and contingency teams, work collaboratively.
The patient is also considered a member of the healthcare team, emphasizing co-construction between the patient and the team rather than doing things solely for the patient.
What are some communication tools and strategies used in healthcare teamwork to improve patient outcomes?
The goal of teamwork is to work together efficiently and effectively to improve patient outcomes.
- TeamSTEPPS employs structured and efficient communication using the SBAR framework: Situation, Background, Assessment, and Recommendation. SBAR ensures essential information is effectively shared in time-constrained situations, improving communication in healthcare.
- Callout is another communication strategy where vital information is audibly conveyed, similar to pilots using “mayday” during emergencies. In the operating room, the anesthetist may call out medication administration to keep everyone informed.
- Check back, based on closed-loop communication, involves repeating and confirming key information, enhancing accuracy.
- Handoff is the exchange of information during care transitions, transferring not only information but also patient responsibility and risk. It allows for questions and clarifications, promoting effective communication during transitions.
In communication, there are three important tools:
- The call-out: It is a strategy used to communicate critical information and draw attention to a crisis or situation.
- The check-back: It applies the principle of closed-loop communication, where messages are repeated and confirmed to ensure accuracy and understanding.
- The handoff: It is the transfer of information and responsibility during transitions of care, and it includes an opportunity to ask questions and clarify any uncertainties.
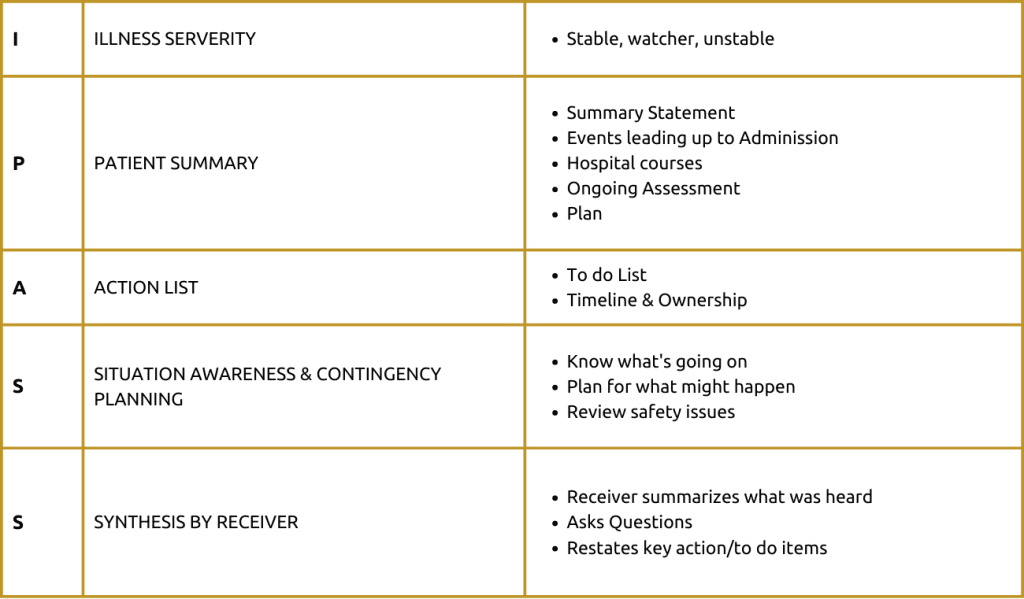
There are two possible tools for structured handovers:
- iPass the Baton
- iPass
In Switzerland, the iPass tool is preferred, a five-step communication tool that categorizes patients based on illness severity, summarizes their status and treatment plan, creates an action list with timelines and responsible parties, anticipates future situations, and rephrases key actions for receivers. By utilizing these communication tools and strategies, healthcare teams enhance patient safety and improve the quality of care provided.
What are the differences between designated leaders and situational leaders in the context of leadership and Team STEPPS?
In the context of leadership and Team STEPPS, there are two types of leaders:
- Designated leaders: Designated leaders are long-term positions such as the chief physician or chief nurse of a ward.
- Situational leaders: Situational leaders are those who take charge in emergencies, such as the first responder to a stroke or cardiac arrest.
Effective team leadership, as outlined in Team Steps, applies to both situational and designated leaders.
TeamSTEPPS offers effective leadership strategies for both designated and situational leaders. The brief tool helps share plans, allocate tasks, and establish safety goals, ensuring everyone is on the same page.
Four leadership tools improve team performance and situation monitoring:
- Building a safety climate: Creating an environment where team members feel safe to speak up and share information, ensuring alignment in content and climate.
- The Brief: A team briefing is an effective strategy for sharing the plan, forming the team, and designating roles, responsibilities, and goals.
- The Huddle: A short ad-hoc meeting to regain situation awareness, discuss critical issues, and reassign resources and tasks within the team, helpful during changing situations.
- The Debrief: Learning from experiences to identify strengths and areas for improvement, facilitating continuous learning and enhancement.
Situation Monitoring
An individual skill to assess the environment and detect emerging situations leads to shared mental models and improved team outcomes when shared with the team.
The suggested model for situation monitoring comprises four steps.
- The first step: Involves looking into the status of the patient.
- The second step: Is to assess the team members’ condition, including their fatigue and stress levels.
- The third step: Involves examining the environment, such as the equipment being used.
- The final step: Is to progress toward achieving the goal.
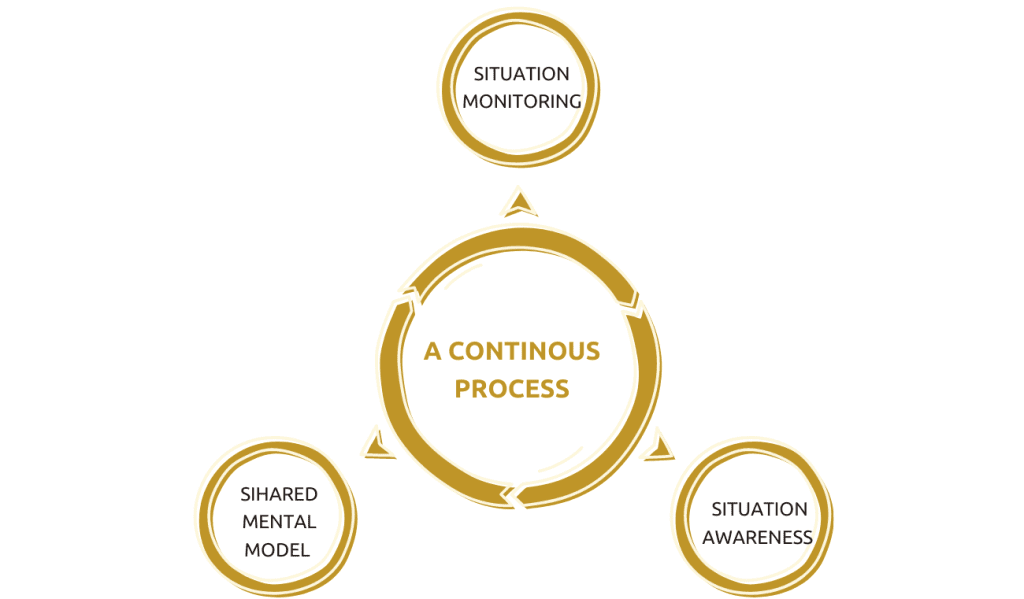
In TeamSTEPPS, situation monitoring is crucial for understanding unfolding situations. For example, a ward leader walking in the hospital corridor would assess the patient’s status, consider team factors like fatigue and stress, and examine the environment before involving the nurse in charge. This highlights the importance of situational monitoring.
The fourth chapter of TeamSTEPPS emphasizes mutual support, where team members assist, provide feedback, and advocate assertively for the patient’s benefit. Here are the key points related to mutual support:
- Task Assistance: Actively seek and offer assistance in a supportive climate, fostering trust among team members.
- The climate of Trust: Build a culture focused on patient safety and teamwork, establishing an environment conducive to task assistance.
- Creating Trust: Utilize briefings to discuss team goals, clarify roles, and establish a common understanding, promoting a collaborative and supportive team atmosphere.
Effective feedback is timely, respectful, specific, and aimed at improvement rather than blame. Additionally, it should be considerate of the recipient.
What is the CUS tool in healthcare, and how does it facilitate communication about safety concerns?
TeamSTEPPS focuses on improving patient safety by addressing barriers to effective teamwork in healthcare. It offers tools and strategies for communication, leadership, monitoring, and mutual assistance to enhance team performance and situation awareness.
The CUS tool prescribes speaking up when a safety issue arises, by using predefined code words, first “I’m Concerned” and, if that is not enough, “I’m Uncomfortable,” and if this does not get the required attention, “I think this is a Safety issue—can we stop and discuss the situation?. The tool encourages open communication about safety concerns, promoting a climate of trust where team members can confidently seek and offer help. The Desk Script tool helps manage and resolve conflicts constructively by de-escalating situations and finding objective solutions.
By utilizing these tools and strategies, healthcare teams can improve patient safety, enhance the quality of care provided, and create a culture that emphasizes patient safety, teamwork, and a shared mental model. Implementing TeamStepps requires an institutional implementation plan and coaching to reinforce and utilize the skills taught to team members.
Studies demonstrate that TeamStepps positively impacts patient safety culture. In a hospital with two maternity wards, implementing TeamStepps resulted in statistically significant improvements in safety and climate dimensions compared to the control ward.
By integrating TeamStepps into healthcare practices, institutions can foster a culture of safety, improve communication and collaboration among healthcare professionals, and ultimately enhance patient outcomes. [1]Staines, A., Lécureux, E., Rubin, P., Baralon, C., & Farin, A. (2020). Impact of TeamSTEPPS on patient safety culture in a Swiss maternity ward. International Journal for Quality in Health Care, 32(9), 618-624.
The study “Impact of TeamSTEPPS on Patient Safety Culture in a Swiss Maternity Ward” by Staines et al. assessed the effects of TeamSTEPPS implementation on patient safety culture. The intervention in one ward led to significant improvements in three dimensions of patient safety culture: Supervisor/Manager Expectations and Actions Promoting Safety, Teamwork Within Units, and Nonpunitive Response to Errors.
These results indicate that TeamSTEPPS can effectively enhance patient safety culture, especially in high-risk settings like maternity wards. Even after accounting for baseline differences, a significant improvement in one dimension remained.
Conclusion
Teamwork and effective communication are vital in healthcare to enhance patient outcomes. While the WHO safety checklist improved certain aspects, it remained uncertain if it significantly enhanced teamwork. To address this, the federation of hospitals adopted TeamStepps which includes communication tools like SBAR, call-out, checkback, and handoff. These tools aim to promote structured communication, efficient information sharing, and patient safety. Recognizing the patient as part of the healthcare team makes healthcare a collaborative effort. Prioritizing teamwork and communication is essential for improving patient outcomes in healthcare.
Author
-

Patient Safety Programme Director, Federation of Hospitals of Canton Vaud, Switzerland



