Patient Safety Culture: Concept, Measurement and Practice
Read the Magazine in PDF
Abstract
Patient safety remains a quality challenge in Canada and many other countries. While many interventions have been developed to address safety challenges, many of these have had limited impact in many settings. The underlying issue limiting improvements in patient safety is patient safety culture. This brief report summarizes the role of patient safety culture, the ways in which it can be measured, and the strategies that can influence culture to inform improved performance. Leaders play a vital role in fostering a culture for effective safety measurement and improvement. Selecting the right tool for measuring safety culture is essential, and there are several tools that have strong measurement properties that have been used to guide improvements.
Introduction
Patient safety remains a persistent global problem despite efforts to address safety gaps. Studies and monitoring in healthcare organizations continue to identify high levels of adverse events. For example, a recent Canadian study identified that one in four ICU patients experienced harm. Implementation and scalability of interventions have also been challenging.
There are a growing number of interventions addressing specific types of patient safety events, such as central line infections or pressure injuries. But substantial barriers to improvement remain, including organizational culture, resistance to change, resource constraints, and limited collaboration among healthcare professionals. There is a growing consensus that technical changes are insufficient without cultivating a culture that supports their use and amplifies their impact.
Patient safety culture
The foundation of safer care is an improved patient safety culture. Patient safety culture enables staff to understand their role and their impact on safety. Encouraging error reporting and building a safe care environment are crucial to identify key themes in creating safer care. Frontline staff need to be supported in their efforts to perceive safety challenges and to promote safer care. Developing a patient safety culture is imperative for a safer healthcare system. There is an expanding knowledge base on the impact of improving patient safety culture on the reduction of patient harm.
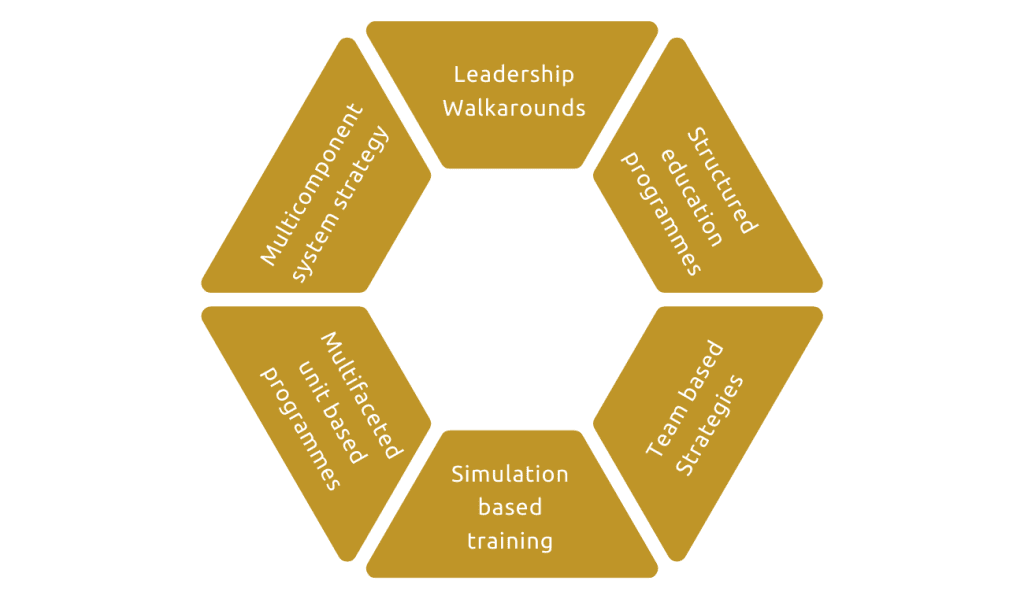
A systematic review titled “Promoting Safety Culture in Acute Care” evaluated initiatives promoting safety culture in acute care settings. Analyzing 33 relevant studies, including interventions like executive walk rounds and team training the authors demonstrated the potential for positive change in safety culture and patient outcomes. However the strength of this evidence was generally low, and further research is needed on more effective strategies for promoting a safety culture in healthcare settings.[2]
The importance of a patient safety culture lies in the shift from a blame culture to a learning culture.
Interventions succeed in Supportive Environments
Patient safety interventions are crucial for improving healthcare, but their effectiveness heavily depends on the environment in which they are implemented. A patient safety culture is essential to providing a supportive environment for these interventions to thrive. There are several key elements of a patient safety culture that promote safe and reliable care. These are:
- Effective teamwork and communication
- Strong clinical leadership
- Local data and accountability
- Understanding quality improvement methods
- Ongoing learning and reflection
- Senior leadership support
These are crucial components of a supportive patient safety culture. Without these elements, patient safety interventions may not be effective in improving care.
Developing a Just Culture
Blaming individuals for errors results in limited reporting, which hinders learning and progress. While individuals commit errors, poorly designed systems often contribute to harm. James Reason, a former psychology professor at the University of Manchester, developed the concept of just culture in patient safety and an accountability framework that helps to distinguish between system issues and individual factors for safety incidents, enabling targeted improvements and avoiding blaming individuals for system failures.
The decision tree tool distinguishes individual responsibility from system issues. For incident review, this approach allows reviewers to assess intentions, deficiencies in training and experience, adherence to procedures, and other relevant issues.
Measuring patient safety culture
To improve patient safety culture, organizations must first measure it. Various measurement tools exist, but translating survey results into action is crucial. Strategies to improve patient safety culture include leadership support, walkarounds, simulation, and building unit capability and interest in reporting and learning from events. Articles by Marella et al. and Sally Weaver review evidence for these strategies. Implementing these tools effectively is essential for patient safety culture improvement. [3]
A short but impactful tool for improving patient safety culture is discussed in an article by Mark Fleming. The tool focuses on several elements closely related to patient safety culture and prompts questions about the maturity levels of leaders, staff, and reporting systems.
4. The Patient Safety Culture Improvement Tool (PSCIT) was developed to help healthcare organizations enhance their safety culture. It includes a safety culture maturity model with five phases of growth.
The PSCIT comprises nine components addressing various aspects of patient safety culture. Organizations can assess their current level of maturity and progress to the next level using the provided descriptions. Due to limited data on reliability and validity, caution is advised when using the PSCIT. [4]
The role of leaders across organizations in measuring Patient Safety Culture:
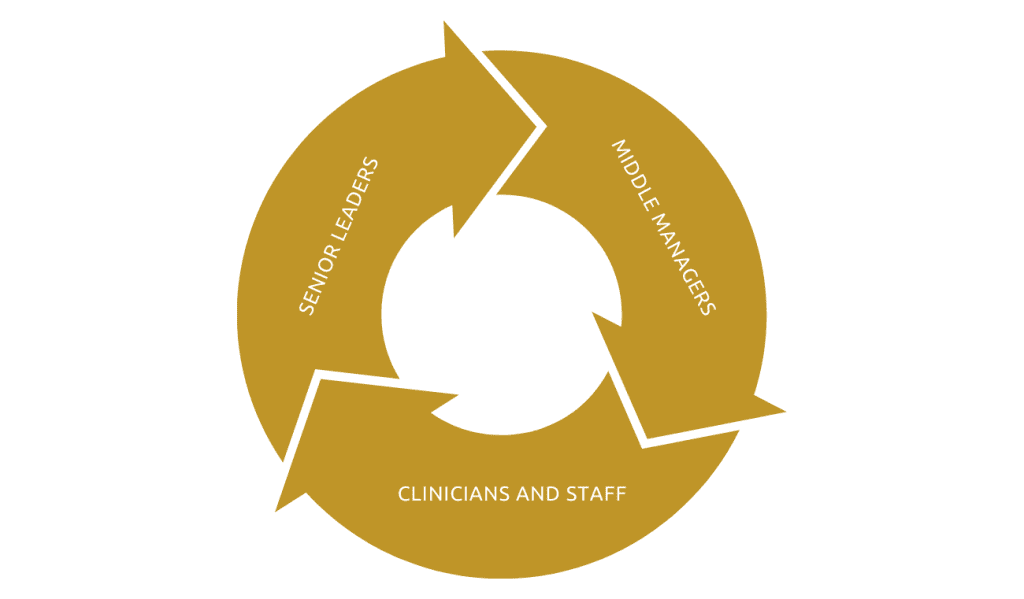
Senior leaders, middle managers, clinicians, and staff all play significant roles in developing and maintaining a positive safety culture. Safety culture measurement is often fragmented, either top-down or bottom-up. Senior leaders establish the framework for developing a positive culture, while middle managers implement strategies and communicate safety issues to frontline staff. In a supportive environment, middle managers act as champions for measurement and culture change, but in an unsupportive setting, they may hinder change. Clinicians and care providers need to understand the importance of a supportive culture.
Patient safety culture tools and surveys
To measure safety culture effectively, the psychometric properties of the survey must be considered, to ensure its validity and reliability.
Selecting the appropriate tool depends on the specific goals of measurement. While the ultimate objective is to enhance safety culture, other purposes like benchmarking or establishing a safety foundation should be considered. The level of engagement desired with the results is also a factor, as some tools allow for more in-depth exploration
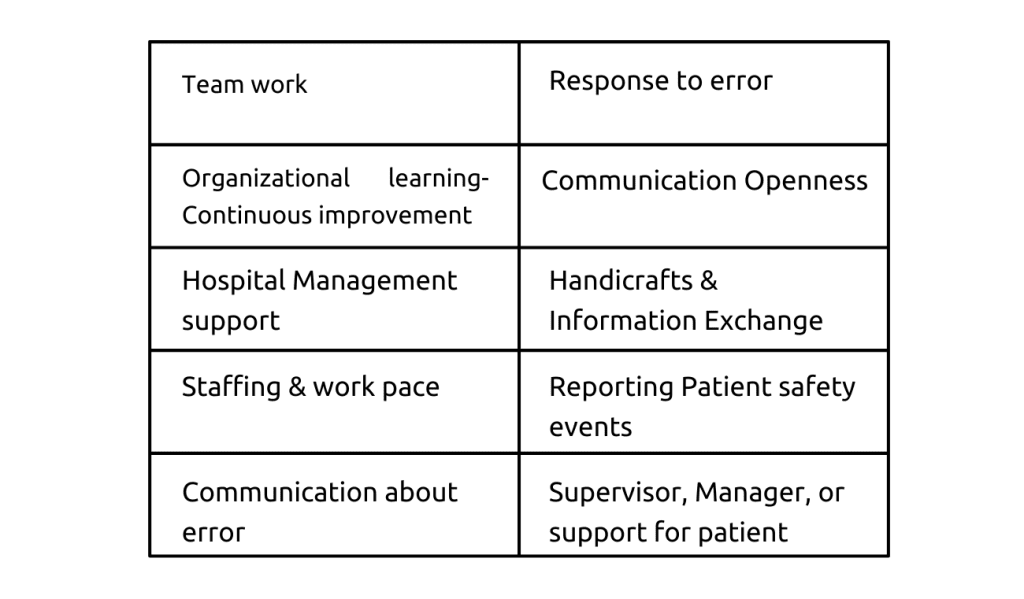
There are several well-validated tools to assess patient safety culture. These include the US Agency for Healthcare Research and Quality survey on patient safety culture, which has been widely used. This survey assesses dimensions such as supervisor support, hospital management backing, response to errors, teamwork, and communication. Its effectiveness depends on how an organization utilizes the survey results.
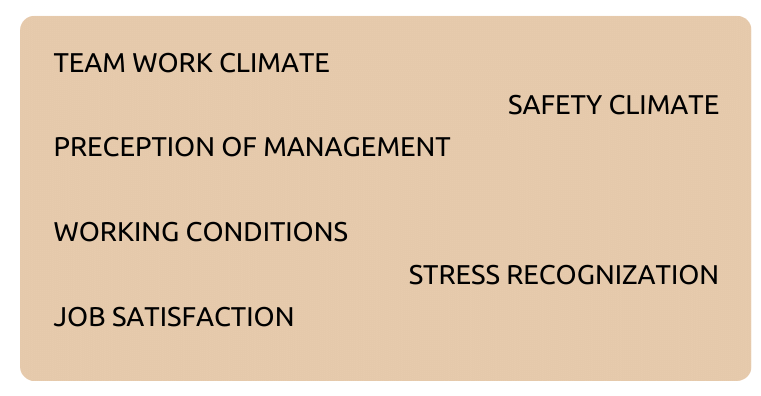
A second tool is The Safety Attitudes Questionnaire, adapted from the aviation industry, which examines six dimensions of patient safety culture and has good psychometric properties.
A third valuable tool is The Manchester Patient Safety Framework, which offers an innovative approach based on five elements of safety and offers a growth model and a roadmap for improvement.
Integrating Patient Safety Culture Measurement and Improvement into a Safety Program
Creating a culture of safety requires both leaders and staff to participate in the measurement process and drive tangible changes. By employing mindfulness and high-reliability organizing principles, organizations can achieve higher-reliability organizing by emphasizing an unwavering focus on safety. Frontline workers become empowered to initiate safety improvements, resulting in a combined top-down and bottom-up approach that reinforces the culture of safety. Utilizing measurement as an intervention strengthens the organization’s safety culture.
The principles of mindfulness and high reliability facilitate the adaptation and impact of patient safety culture efforts.
For those who are unfamiliar with these principles, they consist of five key elements.
- Preoccupation with failure: Identifying potential gaps and weaknesses.
- Reluctance to simplify: Examining assumptions and avoiding oversimplification
- Sensitivity to operations: Paying close attention to the surrounding environment.
- Deference to expertise: Recognizing and leveraging expert knowledge.
- Commitment to resilience: Learning from adverse events and making improvements.
The key message is that measuring patient safety culture should be a fundamental aspect of improving care, not merely a checkbox. Safety practices must be continuously integrated into organizational, clinical, and managerial practices to prevent them from becoming perceived as administrative burdens for staff and managers.
Conclusion
Patient safety requires effective interventions and support for healthcare professionals. Developing a safety culture involves teamwork, communication, leadership, accountability, quality improvement, learning, and senior support. Distinguishing individual responsibility from system issues is crucial, and tools like James Reason’s decision tree can help address unique system needs. Measuring patient safety culture is essential, but improvement depends on the implementation of culture, teamwork, mindfulness, and high-reliability principles. Participation from all individuals is key to creating a strong safety culture, making measurement a core activity in improving care.
References
- Shekelle, P. G., Pronovost, P. J., Wachter, R. M., McDonald, K. M., Schoelles, K., Dy, S. M., … & Walshe, K. (2013). Annals of internal medicine, 158(5_Part_2), 365-368.
- Weaver, S. J., Lubomksi, L. H., Wilson, R. F., Pfoh, E. R., Martinez, K. A., & Dy, S. M. (2013). Annals of internal medicine, 158(5_Part_2), 369-374.
FAQs
Q.How to interpret survey results if staff do not respond to the survey?
A.If staff do not respond to a survey, it can be challenging to interpret the survey results. It is essential to understand why staff are not responding to the survey. If staff do not see the survey as a valuable activity and do not believe that management and clinical leaders will pay attention to it, they may not respond. Therefore, leadership should let staff know why it is important to fill out the survey and how the survey results are influencing decisions within the organization. Once staff see that the survey results are influencing efforts to support frontline staff, they are more likely to respond to the survey.
Authors
-

Professor and founding program lead, Masters of Quality Improvement and Patient Safety, Institute for Health Policy, Management and Evaluation; Dalla Lana School of Public Health, University of Toronto, Canada
-

Dalla Lana School of Public Health, University of Toronto, Canada; Ph.D. Candidate, Institute for Health Policy, Management and Evaluation, University of Toronto, Canada



