Clinical Communication in Challenging Situations
Read the Magazine in PDF
Abstract
The article explores the potential benefits of a person-centered registry-enabled learning health system, including improved health outcomes, healthcare value, and scientific knowledge, through data and conversations. It presents case studies supporting this claim, with a focus on serious illness conversations. The report highlights the importance of patient-provider communication and co-production in healthcare to enhance the patient experience. The Dartmouth project aims to increase the frequency of conversations with seriously ill patients efficiently, utilizing the Serious Illness Conversation Guide.
Introduction
The hypothesis suggests that a person-centered, registry-enabled learning health system can co-produce better health outcomes, improve healthcare value, and advance scientific knowledge through conversations and data. Evidence and cases, focusing on serious illness conversations, support this claim. Prioritizing better conversations within a learning health system is crucial for success, akin to “skating to where the puck is going to be,” as Wayne Gretzky famously said. A case study from Dartmouth, featuring the founders of the Spine Center, highlights their novel approach to holistic spine care through an improved information ecosystem and communication.

Tracking outcomes for individual patients
At the Spine Center, a health assessment is completed to gauge current health status and care expectations. The data are summarized and transmitted to the clinician, facilitating targeted discussions on the condition, treatment options, and preferences. A dashboard, generated within 20 minutes, reviews medical history, risk factors, symptoms, and quality of life outcomes, comparing them with desired expectations. This innovative learning system integrates with a registry shared by twelve other centres, enabling analysis at individual and population levels. Patient-reported data fosters better conversations and continuous improvement in care.
The value compass compares the outcomes of patients with herniated discs who underwent surgery or non-surgical care across twelve centres. Surgical patients showed better clinical results, functional outcomes, and satisfaction but incurred higher total costs. The use of patient-reported outcomes helps calculate individual patient values, informing real-time care decisions. A personalized risk calculator aids in deciding between surgery and non-surgical care, showing higher chances of improvement with surgery. The learning system has led to over a hundred publications and exemplifies co-producing better health through a learning system approach.
Patient-physician partnership
In the year 2000, Dr. Staffan Lindblad visited the Dartmouth Spine Center and saw the potential to replicate it in Sweden. At the Karolinska Institute, he emphasized the partnership between patients and healthcare providers, focusing on effective communication. This led to a learning system for co-producing better health outcomes through improved conversations, resulting in over a hundred publications and ongoing work. Swedish rheumatology practices now use health assessments for patients with rheumatoid arthritis, generating self-management modules that track pain points and disease activity. This exemplifies the power of partnership and communication in healthcare.
In Sweden, the clinician module transmits patient data to clinicians, allowing them to view clinical and patient-reported outcomes and medications over time. The approach has halved disease activity rates in rheumatoid arthritis patients, leading to better outcomes and improved patient engagement. In Gavle County, this system yielded even better results, with disease activity becoming more stable and generally improved. The approach fosters a partnership between patients and clinicians, promoting better self-care and overall healthcare outcomes.
The brainstorming session led to a patient-centered learning health system model for co-producing better health outcomes. The partnership between patients and their families, clinicians, and care teams, works together in an enriched information environment. The system includes patient support networks, a collaborative improvement and research network, and a registry providing data feedback for optimal care. This co-production learning health system aims to achieve optimal health and high-value healthcare through better conversations, reducing wasteful spending, and improving research efficiency.
To improve a patient’s health and well-being, the following steps are essential.
- Co-assess the patient’s health status and impact of the treatment plan.
- Co-decide on the next steps for treatment based on relevant evidence.
- Co-design the treatment plan with the patient to minimize the burden of treatment.
- Co-deliver the treatment plan, involving daily self-management and occasional visits to the clinician. [1]Nelson, E. C., Dixon-Woods, M., Batalden, P. B., Homa, K., Van Citters, A. D., Morgan, T. S., … & Lindblad, S. (2016). Patient focused registries can improve health, care, and science. Bmj, 354.

These registries have had significant impacts, such as facilitating public reporting, research, professional development, and service improvement. They also highlight variations in practices, processes, and outcomes, identifying areas for improvement. In the US and UK, they have contributed to improvements in managing cardiovascular disease and stroke, cancer, and joint replacement.
This model is being implemented across various populations in the United States and beyond. At the core of this conceptual model are two key ideas:
- Co-production
- Learning health systems
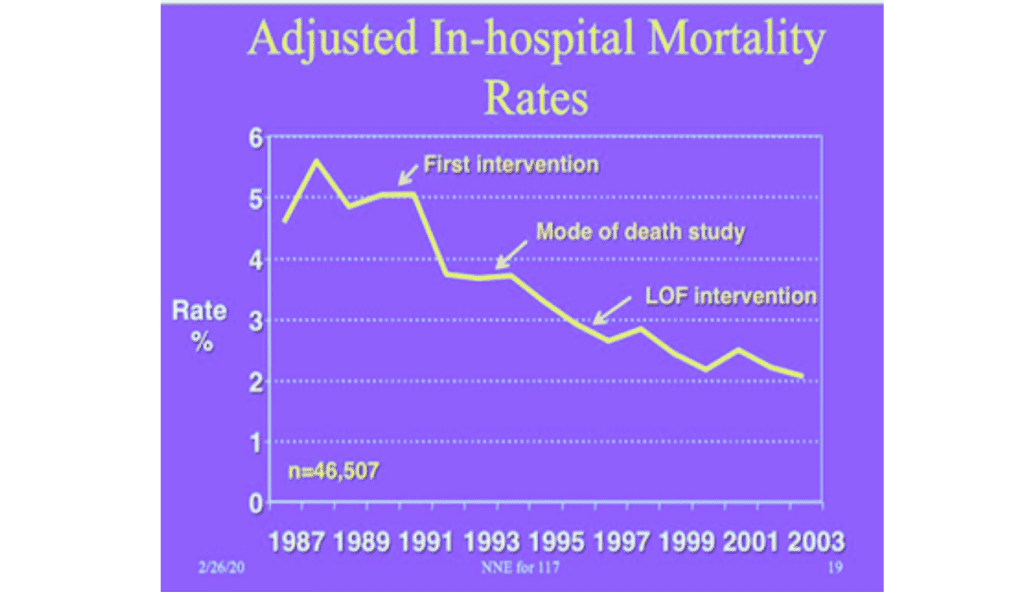
In just a span of eight years, the Northern New England Cardiovascular Study Group was able to decrease open heart surgery mortality rates from about 4.5% to 3.5% between 1987 and 1995.
This trend continued through 2003 and beyond. This is just one of the earliest examples of the success of this approach. Another example is the Cystic Fibrosis Learning System, which resulted in a 10-year gain in life expectancy from 1990 to 2012. The Swedish Rheumatology Quality Register is yet another success story, with a continued downward trend in disease activity up to 2017. Dr. Cullinan will now take over to discuss this approach and crucial conversations in greater detail, specifically focusing on her work in the cancer center at Dartmouth.
Collaborative Learning Network
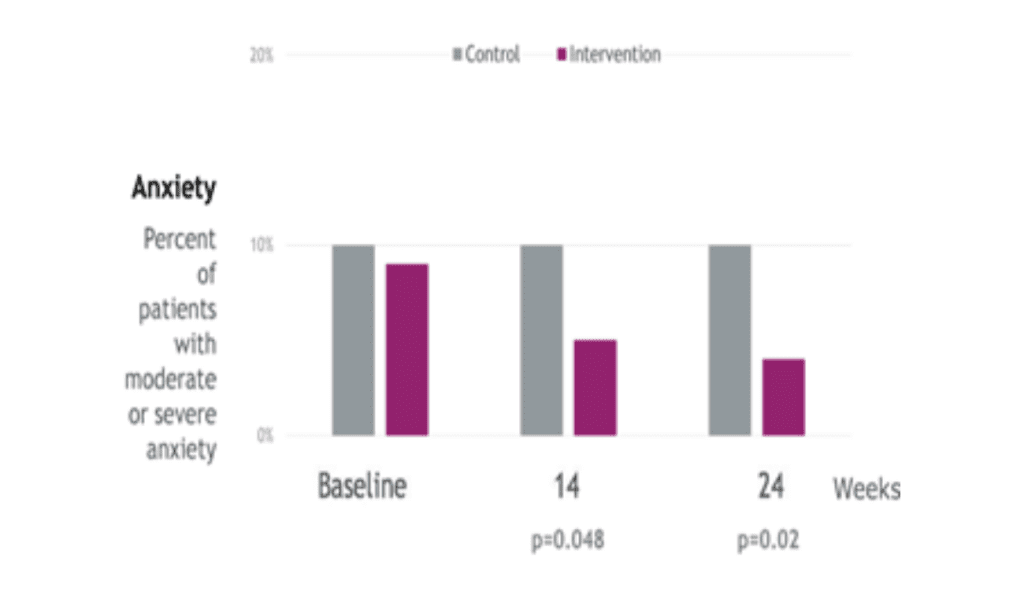
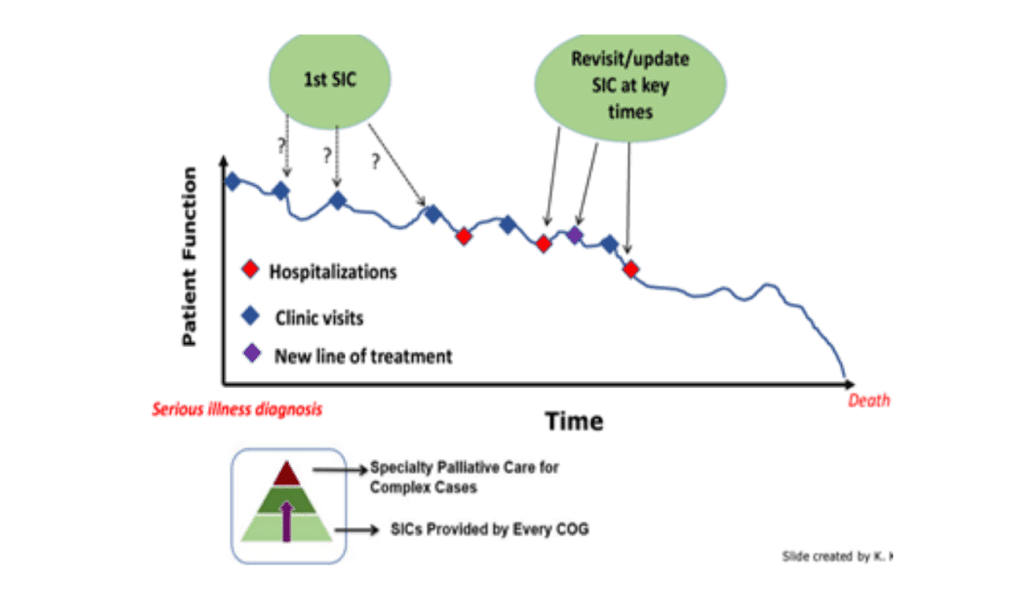
The collaboration between The Dartmouth Institute and powerful organizations aims to enhance the patient and healthcare team experience by co-designing care with patients and families. The focus is on the Serious Illness Conversation, part of a broader initiative that includes Patient Wisdom, Point-of-Care Dashboards, Support Networks, Data Measurement, and a Learning Network. The Serious Illness Conversation Guide, developed by Ariadne Labs, helps clinicians elicit patient values and goals earlier, leading to increased frequency and documentation in the EMR. Contrary to concerns, using the guide reduces patient anxiety and results in meaningful behavioral changes that extend beyond medical care. Patients value these discussions for their impact on their personal lives as well.
The Dartmouth project aims to increase the frequency of conversations between oncology teams and seriously ill patients, initiating them before complications arise.The guide facilitates efficient and high-quality conversations, with median times of
22-26 minutes. Sharing the conversation’s work among the healthcare team, including billing possibilities, enhances efficiency. Centralizing documentation in the electronic medical record further streamlines the process, making patient goals and values easily accessible during admissions. The goal is to implement this approach center-wide, starting with specific specialties and expanding gradually. Efficiency is a key factor driving success in the healthcare system.
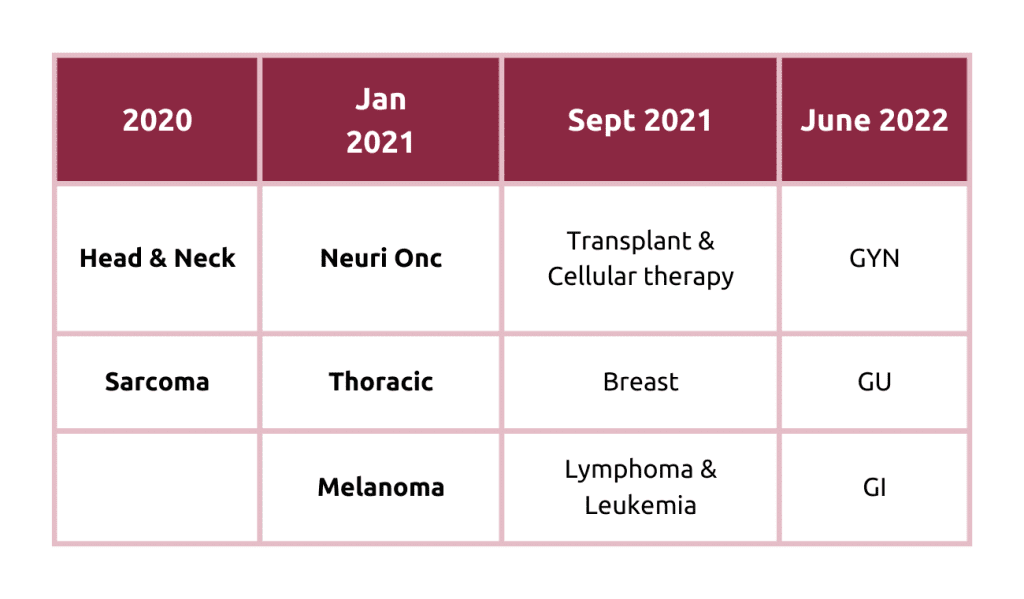
The initiative aims to improve the quality of serious illness conversations by oncology teams, and the timing: for some patients, that may be as soon as within the first three to four visits after diagnosis. This approach expands access to the conversation for more patients but also permits referral to palliative care services for complex cases. Implementation focuses on education and making these conversations standard practice. A multidisciplinary team, including a patient and family advisor, was trained in serious illness conversations, emphasizing the importance of these discussions. Coaching, co-designed eligibility criteria, and workflow improvements were used to integrate conversations seamlessly into the healthcare team’s work. The learning health system will guide ongoing efforts to meet patients’ and providers’ needs effectively.
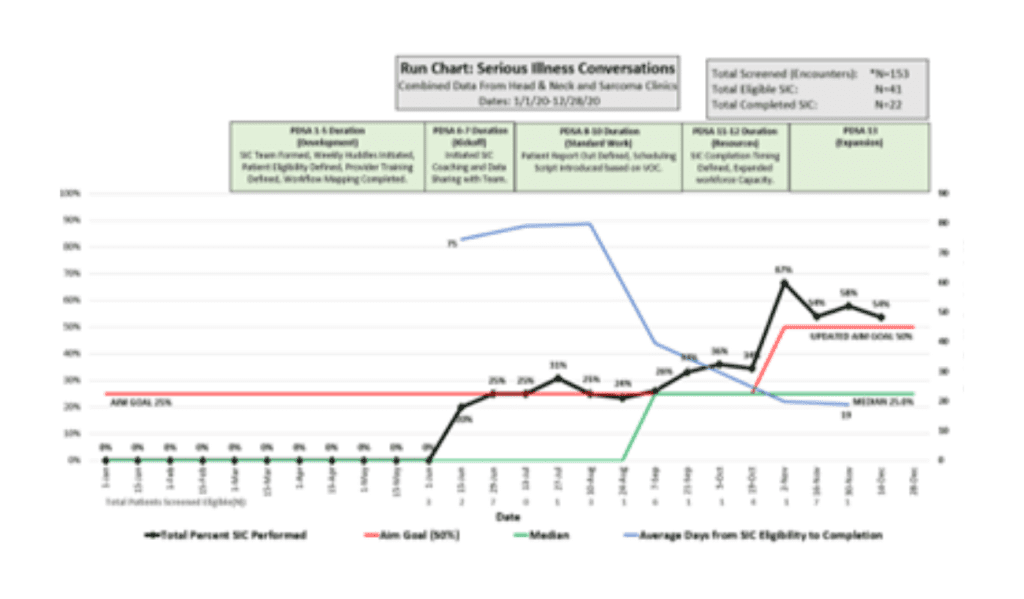
The Cancer Center’s head and neck and sarcoma departments tracked progress in serious illness conversations from January to December 2020. The aim was to increase completed conversations, with an initial goal of 25% (red line). Through PDSA cycles, workflow improvements, coaching, and patient involvement, the percentage increased to 67%. Sustaining progress is now the focus, with conversations becoming a cultural norm.
The team participated in a learning collaborative, reflecting on their work and sharing lessons learned.
Some of the learnings from the head and neck and sarcoma teams included:
- Family advisor involvement reduced barriers to starting conversations with patients on sensitive topics.
- Conversations earlier in the process increased clinicians’ confidence in delivering high-quality care.
- The experience reframed clinicians’ perspectives on their role, focusing on patients’ values and priorities.
- Being part of a learning health system fosters a sense of team equity, a growth mindset, and increased engagement.
Conclusion
Evidence from various healthcare settings supports the person-centred registry-enabled learning health system. Examples include using patient-reported data to personalize care and improve outcomes at Dartmouth Spine Center and Swedish Rheumatology Quality Register. The Northern New England Cardiovascular Study Group reduced mortality rates through collaborative learning networks. The Serious Illness Conversation guide increases conversation frequency, reduces anxiety, and drives behavioural changes. Implementation involves a multidisciplinary team, prioritizing efficient, high-quality, and rewarding conversations. This approach enhances healthcare value and scientific knowledge, improving health outcomes.
Authors
-

Prof. Community & Family Medicine The Dartmouth Institute for Health Policy and Clinical Practice
-

Assistant Professor, Medicine, The Dartmouth Institute for Health Policy and Clinical Practice



