Person-centered care and its principles
Read the Magazine in PDF
Abstract
The objective of the project outlined in this article is together with the International Society of Quality in health care (ISQUA), to create awareness about person-centered care (PCC) and encourage its implementation in healthcare systems through the publication of a white paper on PCC. [Bohren, M. A., Vogel, J. P., Hunter, E. C., Lutsiv, O., Makh, S. K., Souza, J. P., … & Gülmezoglu, A. M. (2015). The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS medicine, 12(6), e1001847.]
The CAHO talk’s starting point is how care that is not respectful of the patient’s needs, values, and preferences, can sometimes disintegrate into care that is experienced as rude, disrespectful, and abusive. One example comes from a paper on women giving birth in healthcare facilities in India, Ghana, and Kenya, where 16% of the women reported verbal abuse during their stay in the hospital, and 73% of Indian women reported that providers did not ask permission before the performance of a medical procedure [1]. The study employed a mixed-methods systematic review to establish an evidence-based categorization of experienced mistreatment women choosing to give birth in health facilities. The consequence of such experiences may be a reluctance to choose birth in a healthcare facility again, which puts both mothers’ and children’s health and well-being at risk. While this documents a widespread and systematic problem across the globe in maternal health, the problem is found in every corner of modern health care.
The white paper delves into the distinct aims of the three stakeholders in healthcare: the payer, the patient, and the professionals.
Additionally, it underscores the significance of acknowledging the intricacy of healthcare systems and adopting new language that integrates patient objectives into the care system to achieve person-centered care.
Introduction
ISQUA has invited a group of patient partners, led by Prof Berntsen, to contribute to a white paper on person-centered care for ISQua. The purpose of the white paper is to function as a manual for healthcare managers, professionals, and patients worldwide. The project’s objective is to create awareness, foster comprehension, and prompt contemplation of the significance of person-centered care, its constituents, and its implementation in care systems.
What is PCC?
Defining person-centered care remains a challenging task despite several reports advocating for it since the 1930s, as per a UK Health Foundation report.
A recent definition of person-centered care has been published by the American Geriatrics Society Expert Panel.
This definition consists of two points:
- The first describes what person-centered care is.
- The second explains how to achieve it.
Person-centered care involves recognizing an individual’s values and preferences that guide all aspects of their healthcare and requires collaboration among the individual, significant others, and healthcare providers to make informed shared decisions that align with the individual’s desires.
In the context of ISQua, the group recognizes that every patient is a unique individual with a personal background that shapes their life goals and priorities. Their healthcare journey becomes crucial if a health problem threatens their personal goals. In this context, the healthcare system’s role is not to simply cure the health challenge, but rather to aid the individual in achieving their meaningful life goals, without unnecessary disruption of their life project. Providers go from being “we know best”, to a partnership, where providers and patients, through shared decision-making, co-design the patient journey.
Therefore, ISQua prioritizes person-centered care by focusing on the person’s life goals and providing support accordingly. The group stresses the patient journey in person-centered care, where patients’ priorities guide care decisions. Patients and professionals work together to co-create the journey to achieve the patient’s meaningful goals within the healthcare system’s constraints.
Why is PCC so difficult?
Although patient-centered care is commonly emphasized in management documents and white papers, patients frequently report feeling neglected and mistreated within the healthcare system. The challenge is to comprehend why patient-centered care is not yet the norm. To do so, it is necessary to acknowledge that our actions often align with the objectives of the system in which we work. What are the healthcare system’s objectives? While they may be expressed as patient-centered, our conduct may indicate otherwise. To fully comprehend the healthcare system’s objectives, it must be viewed as a whole.
Healthcare systems aim to improve the well-being of the population they serve by enhancing health, which is defined by the World Health Organization as a state of complete physical, mental, and social well-being.
Health is a positive concept that includes personal and social resources, in addition to physical capacities. The goal of healthcare is not limited to providing technically excellent care, but also to enhance the smallest unit of care, which is the consultation, and align with the principles of person-centered care.
The care system involves the professional, the patient, and the system itself, consisting of various decision-makers. The patient’s journey through the healthcare system involves multiple interactions with various professionals, making the consultation only a part of their journey. By breaking down the care system into roles and structures, we can better understand how it works. The patient journey occurs at the meeting points between the patient and the professionals, with the desired outcomes being improved patient experience, health, and function, professional satisfaction, and cost-benefit ratio for the care system/payer. It is crucial to understand this background when considering,person-centered care as all three roles involved in every patient journey matter and have their significance.
The three roles involved in healthcare –
- The payer/ Governance
- The patient
- The professionals
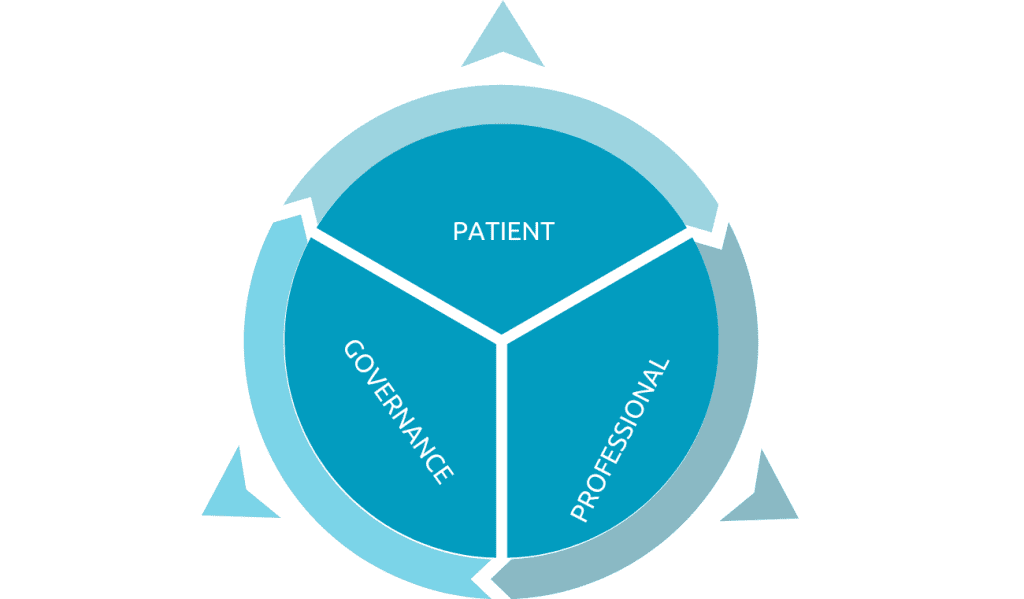
The patient, healthcare professionals, and the care system/payer have different objectives when it comes to pursuing better health. Patients prioritize their life goals, while healthcare professionals focus on improving their patient’s health and function. The care system/payer aims to enhance the health of the population, which may not consider the individual patient’s perspective. This can lead to conflicts between the goals of healthcare professionals and the constraints imposed by the care system.
Two lines of logic clash in healthcare:
- The goal of the person
- The goal of the system and professionals
Professionals and the system prioritize technical excellence, cost-effectiveness, and outcomes defined by professionals, which can overlook patients’ personal preferences, values, and needs.
Patients have the right and responsibility to take care of their health within their context and life project, but their voice is often overlooked due to their weaker position in terms of power and resources. This makes person-centered care challenging to achieve.
Why does PCC make sense?
The demographic change towards longevity causes a shift towards a higher prevalence of chronic conditions and long-term healthcare needs.
Patients with chronic conditions and multimorbidity account for the majority of healthcare costs, highlighting the importance of working with patients to improve outcomes and reduce costs.
In the context of a chronic condition, life, and health care gets to be woven together. In chronic conditions, the person is the defacto carer 99,9% of the time. It is essential that we partner with patients to help them manage their own care. Collaboration with patients is necessary to address the increasing prevalence of long-term conditions in India and globally. Without mutual respect, this collaboration will falter. PCC is a road to achieving the trust and foundation for long-term self-management of chronic conditions.
Why is PCC important?
Delivering excellent technical care and showing empathy should not conflict but go hand in hand to provide comprehensive and compassionate healthcare. These examples emphasize the need to prioritize person-centered approaches to improve patient experiences and overall healthcare outcomes.
Case Study
1. Bohren et al. conducted a mixed-methods systematic review that aims to develop an evidence-based typology of the mistreatment of women during childbirth in health facilities.
A total of 65 studies from 34 countries were included, and qualitative findings were organized into seven domains. Quantitative data were described due to heterogeneity. The typology highlights mistreatment at the interaction, facility, and system levels. The researchers recommend adopting this typology for describing the phenomenon, developing measurement tools, and guiding future research and interventions. [Bohren, M. A., Vogel, J. P., Hunter, E. C., Lutsiv, O., Makh, S. K., Souza, J. P., … & Gülmezoglu, A. M. (2015). The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLoS medicine, 12(6), e1001847.]
To answer that question, it’s essential to take into account the intricate nature of healthcare systems such as follows;
- Healthcare systems are complex, and understanding this complexity is crucial for successful change management
- There are three types of problems in healthcare: simple, complicated, and complex
- Simple problems have a well-understood cause-and-effect relationship and straightforward solutions
- Complicated problems have many decision points, but guidelines and expertise can help address them
- Complex challenges, such as childcare, cannot be solved with a standardized pathway and require experimentation and iterative trial-and-error
- Chaos is the final part of complexity theory and can occur during crises and catastrophes, where all rules are disregarded.
-
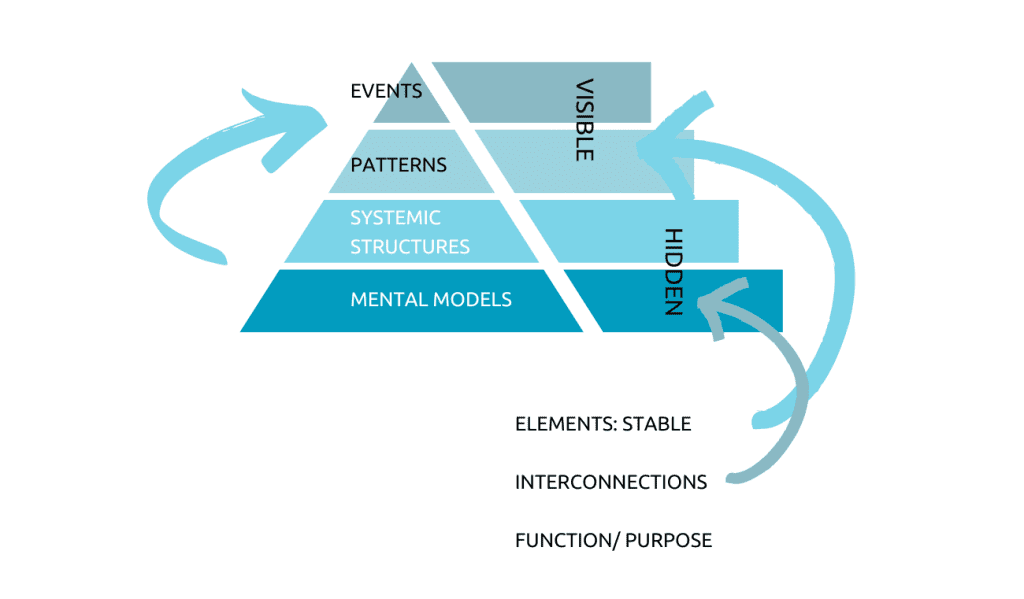
The iceberg model sheds light on the underlying factors driving events in complex systems.
How can we change?
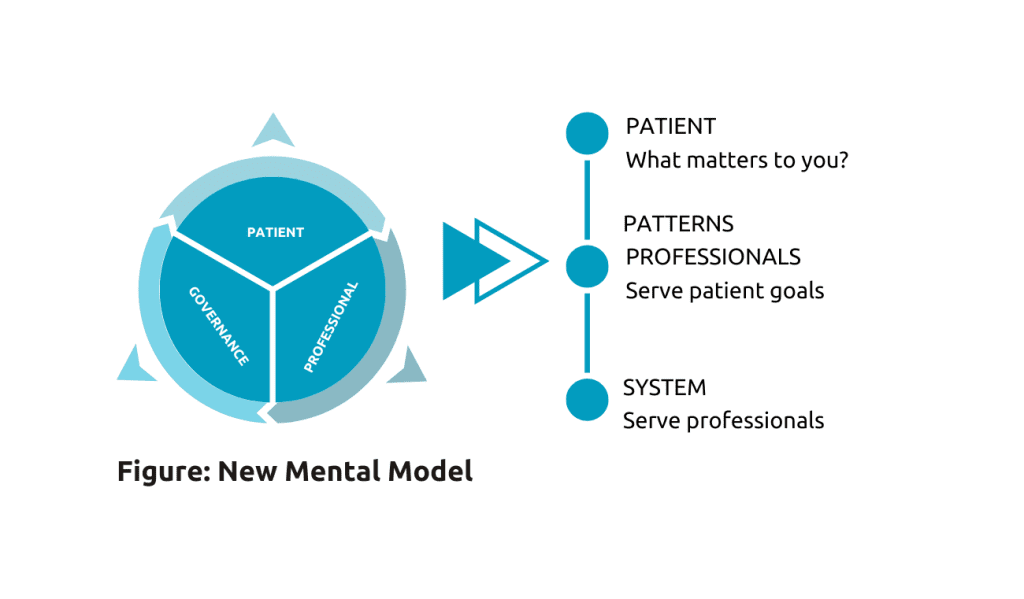
While events and patterns are observable, the systemic structures and mental models driving these patterns are the interconnected elements linked to a function or purpose. For example, a patient’s decision to stop attending his HIV-treatment program due to an experience of abusive behavior or a mother’s feeling of being disrespected are observable incidents. Addressing the systemic structures and mental models behind these incidents is necessary to create a more person-centered healthcare system.
The healthcare system currently prioritizes payers and governance over patient concerns, despite professionals’ efforts to consider patients. The goal is to shift this hierarchy by making patient goals the top priority, with professionals serving those goals and the system serving the professionals. Incorporating patient goals into our language and care system is crucial for achieving this new mental model, which includes identifying the person, understanding their health challenge, and translating their goals into personalized care.
Providers serve as travel agents, tailoring the journey to the patient’s needs, while feedback loops track progress and assess whether goals are being met. Patient experiences should be directly asked about to achieve shared decision-making, and the patient journey should be looked at holistically to identify gaps, challenges, and contradictions.
Person-centered care and integrated care are often discussed together, but it’s important to understand that they are distinct, but interdependent concepts. Person-centered care involves identifying a person’s goals and tailoring care to meet those goals, while integrated care involves coordinating efforts across different healthcare professionals and organizations to the multiple challenges of the patient. By focusing on a person’s overarching goal, healthcare professionals can work together to achieve sub-goals for each stage of the patient journey, leading to integrated care. Person-centered care also encourages proactive care as PCC recognizes the individual’s responsibility and ownership of their own health, and therefore also their critical role in their own care.
Measures and documentation of the PCC
To measure and document person-centred care, a simple form can be used that centers around the question, “What matters?”
Patients may need help rephrasing the question in order to discuss their goals. The “outcomes rating scale” measures the patient’s experience of the consultation using a visual analog scale to measure success [Gibbons, C., Porter, I., Gonçalves-Bradley, D. C., Stoilov, S., Ricci-Cabello, I., Tsangaris, E., … & Valderas, J. M. (2021). Routine provision of feedback from patient‐reported outcome measurements to healthcare providers and patients in clinical practice. Cochrane Database of Systematic Reviews, [10].
Another approach, “Meaningful and Measurable,” focuses on qualitative language data and encourages healthcare workers to explore what matters to the patient, plan together, carry out the plan, and evaluate and learn from the experience. Another tool that might be useful is the Collaborate tool by Glynn Elwyn. [Forcino, R. C., Barr, P. J., O’Malley, A. J., Arend, R., Castaldo, M. G., Ozanne, E. M., … & Elwyn, G. (2018). Using Collabo RATE, a brief patient‐reported measure of shared decision making: results from three clinical settings in the United States. Health Expectations, 21(1), 82-89]

Conclusion
Person-centered care (PCC) is a healthcare approach that prioritizes the individuality, values, preferences, and goals of patients, promoting compassion, empathy, and respect for human dignity. It involves collaboration between patients, healthcare professionals, and significant others, and is crucial for addressing the changing healthcare needs of an aging population with long-term conditions. The ISQua white paper provides guidance for healthcare managers, professionals, and patients worldwide, emphasizing the importance of PCC and encouraging reflection on its implementation. Achieving PCC involves identifying patient needs and goals, creating feedback loops to track progress, and promoting proactive care through patient ownership. While challenging, PCC is necessary for the future of healthcare.




