Clinical Audit and its relevance to outcome measures
Read the Magazine in PDF
Abstract
The clinical audit is a vital process in healthcare. It helps healthcare providers evaluate the quality of care given to patients in comparison to best practices and pinpoint areas where improvements are needed. This article describes the clinical audit process and its role in linking measured outcomes with the evidence base. The article will focus on the UK’s experience with clinical audits and provide insights into the lessons learned from a national clinical audit program in Saudi Arabia.
Introduction
What is a clinical audit?
A clinical audit is a quality improvement process that seeks to improve patient care and outcomes through a systematic review of care against explicit measures and the implementation of change [National Institute for Clinical Excellence. Principles for best practice in clinical audit. Abingdon: Radcliffe Medical Press;2002]. Thus, clinical audit requires systematically measuring patient care and outcomes using explicit methods and implementing changes if needed for improvement.
Clinical audit as a quality improvement process
Flow chart of the clinical audit process:
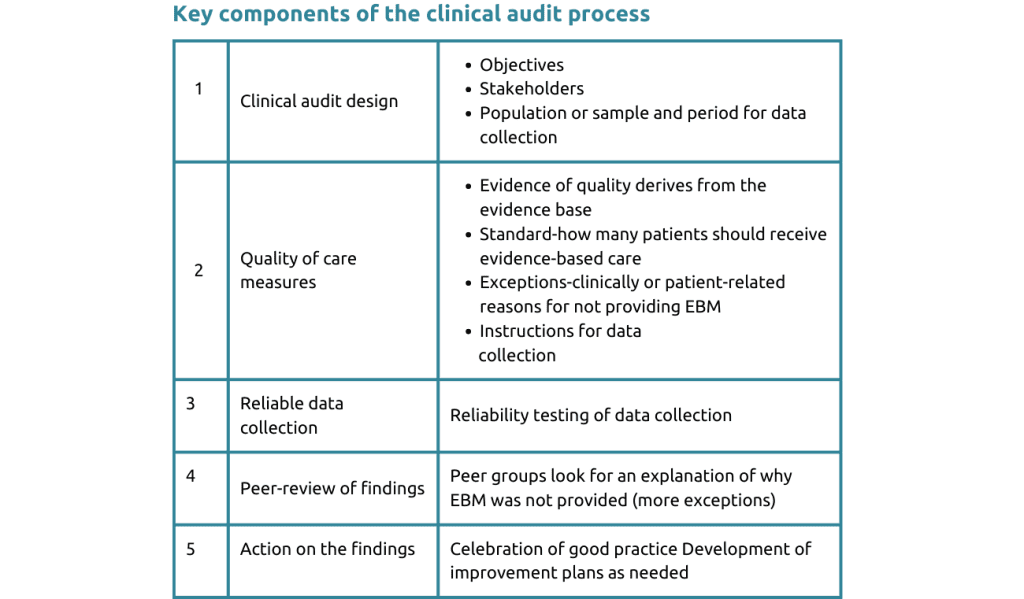
The clinical audit process involves: selecting a subject and defining the purpose of the audit, identifying evidence-based practices, collecting data to assess current practices, making decisions based on findings, celebrating positive results, and implementing improvement plans for challenges or problems in quality. Quality improvement is integrated throughout, and repeating the data collection may be necessary for significant changes or ongoing quality assurance.

Linking measuring outcomes and the evidence base
Clinical audits link directly to the evidence base, systematically reviewing care to enhance patient outcomes. Best practices are measured using evidence-based approaches. Data collection allows providers to assess practices and identify areas for improvement.
Regular audits are needed to sustain excellence and adapt to changes. Addressing issues and implementing improvement plans are crucial. Repeating evaluations ensures effective enhancements. The goal is to improve care quality and patient outcomes.
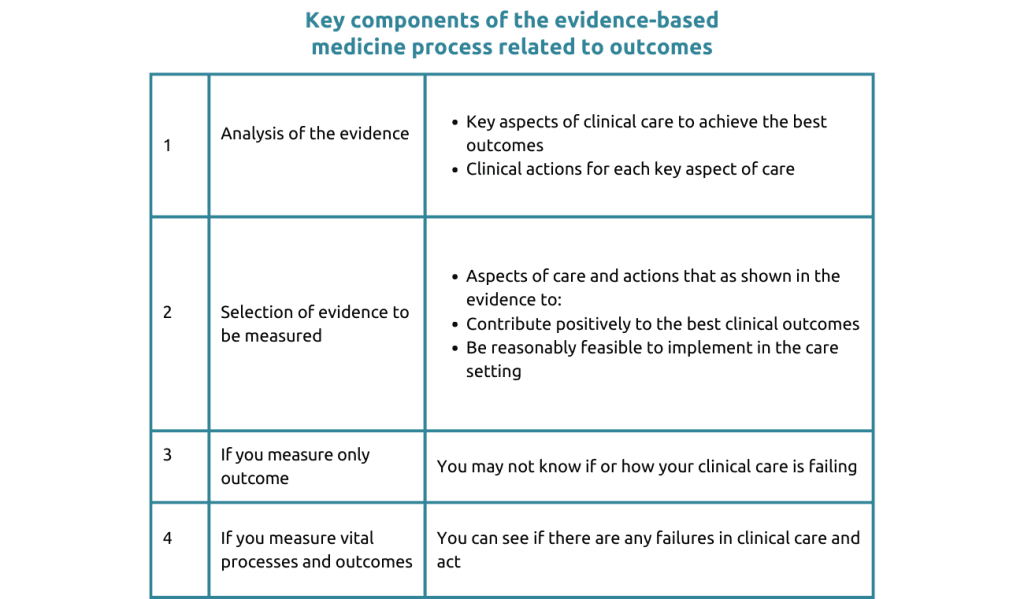
Clinical audits improve care quality through reliable data and evidence-based practice. Measuring outcomes is complex but reveals influential patient factors, which may be recognized through exceptions in the audit measures. Feasible evidence-based practices aid implementation.
Identifying areas for improvement and targeted interventions enhance patient outcomes. Understanding critical procedures helps address care delivery shortcomings.
Understanding UK’s National Clinical Audit Program
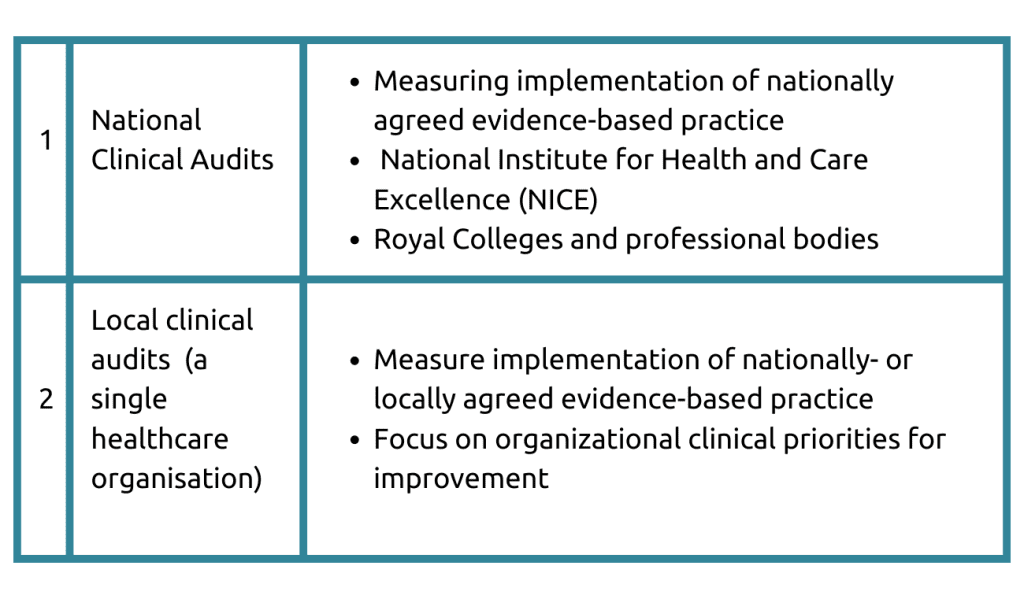
The UK’s National Clinical Audit Program improves healthcare outcomes nationally and locally. It prioritizes areas for improvement through evidence-based practices. National audits target overall improvement, while local audits address specific provider needs. The focus is on critical procedures and achieving optimal patient outcomes.
Following is the list of all the national clinical audit centers for various disease conditions: Arthritis, Asthma & COPD, Bariatric surgery, Breast cancer, cancer diagnosis, Cardiac arrest, Child health outcomes, Child mortality, Cleft, Cystic fibrosis, Dementia, Diabetes, Electric surgery, Emergency laparotomy, End of life care, Epilepsy & seizures, Falls and Fragility fractures, Gastrointestinal cancer, etc.
Funding for the program comes from government, professional groups, and charities. It operates nationally and locally. National audits target broad improvement areas, while local audits address specific organizational needs.
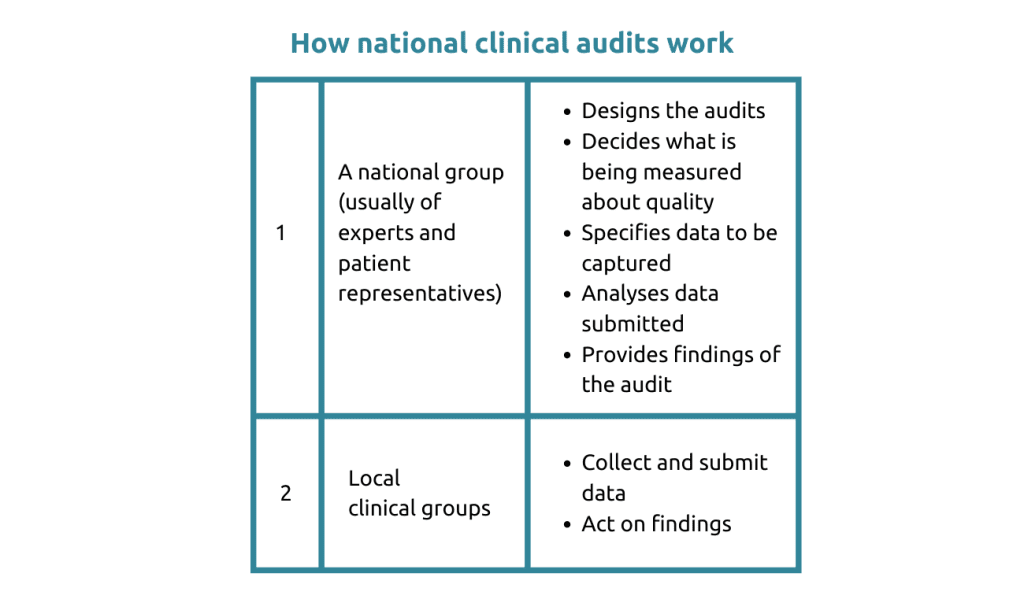
UK’s national audits involve experts and patients collaborating to measure care quality for specific conditions. Some focus on specific outcomes, while others cover broader areas like joint replacements or mental health. Topics include medical, surgical, maternal, and mental health outcomes. Organizations receive reports to enhance treatment based on data analysis.
Examples of the impact of national clinical audits
- The mortality rate of babies undergoing cardiac surgery has halved in 10 years
- Access to specialist stroke units has increased and mortality, length of stay, and rates of institutionalization following stroke all have decreased
- Substantial improvements have been made in access to clinical resources for children with epilepsy in 2 years
- 79% of patients with heart attacks were treated within 150 minutes and 90% were treated within 90 minutes of arrival
- Between 97.4% ad 98.5% of Parkinson’s patients are reviewed clinically each year
Examples of the impact of local clinical audits
- All staff learn about measuring and improving the quality of patient care
- Each clinical service takes responsibility for what needs to be audited and improved
- Every healthcare organization is accountable for measuring and improving quality
- Every doctor is required to participate in clinical audits and quality improvement to be revalidated as a doctor (every 5 years)
- Numerous examples of improvements in patient care at the local level.
NHS standard contract- References to clinical audit (The provider must…)
At the local level:
- Implement an ongoing program of clinical audits of the services provided
- Provide to a commissioner the findings of any clinical audit requested
- Act on recommendations in clinical audits
- Some “audits” are specified such as safeguarding patients, training staff, and protecting clinical information
At the national level:
- Participate in designated national clinical audits
- Make national clinical audit data available to support national publications
In the UK, healthcare organizations must conduct mandatory clinical audits. Personnel participate in the process to assess care quality. Each service performs annual audits based on its priorities. Senior management conducts appropriate audits and implements findings. Clinical audits are compulsory for doctors in training and extended to other healthcare professions.
Quality Account
A quality account is an annual report to the public from a provider of NHS healthcare
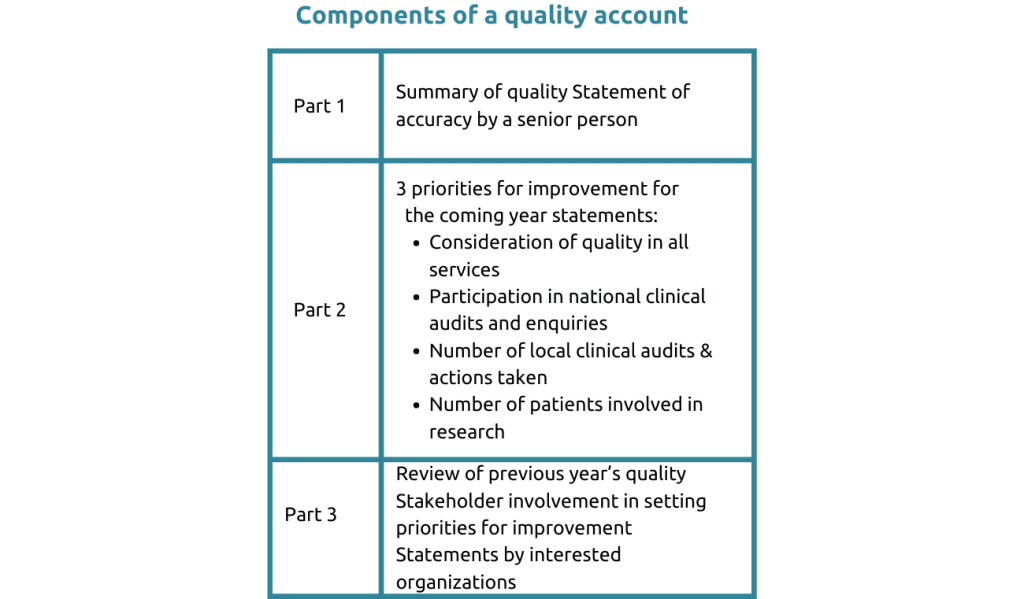
Clinical audits are essential in the UK healthcare system, emphasized through the regulation of healthcare organizations and revalidation for doctors, resulting in local team improvements. National audits are mandatory, overseen by local oversight bodies. Quality accounts from NHS service providers mandated since 2009, focus on care quality, include clinical audits, and are publicly available.
Clinical audit is a valuable quality improvement process
Clinical auditing is vital in the UK healthcare system, improving care through evaluation and interventions. National audits exemplify leadership in quality improvement, incentivizing participation. Standards on designing and conducting national clinical audits published by ISQua guide audits in the UK, Scotland, and Australia. The Care Quality Commission oversees the program, integrating it into regulatory inspections. Local organizations must act on findings, embedding the process into their culture through staff training and accountability, which is assured by independent oversight bodies.
Lessons learned from national clinical audits in Saudi Arabia
Clinical audits are integral to UK healthcare, involving stakeholders in prioritizing improvement areas. In Saudi Arabia, national clinical audits focused on major causes of death or disability, identified best practices from international guidelines, & compared actual hospital practices to best practices through data collected & interpreted for the hospitals.
National clinical audit pathway
Clinical audits are essential in Saudi Arabia for evaluating and improving healthcare quality. Standards were established based on high-quality care criteria, linked to patient outcomes. Hospitals underwent workshops and training, conducting audits to collect data. Iterative improvements followed the data analysis, emphasizing evidence-based practices, data reliability, and multidisciplinary care. Collaboration among healthcare professionals aims to enhance patient outcomes and ensure feasible implementation across different settings.
Clinical care standards
Clinical care standards clearly describe evidence-based care for specific conditions. The approach focuses on aspects closely linked to optimal outcomes, involving diverse healthcare professionals in development and implementation. This has improved patient care quality nationwide.
Developing clinical care standards
- Clinical experts from Saudi selected by the model of care program
- International experts
- Delphi process used with experts to agree on 10 to 15 priority standards
- Content and face validity provided for standardized format for presenting clinical care standards
- Each standard includes:
- Purpose in simple language
- Explanation of key terms in simple language
- Benefits for patients, clinical staff, and the hospital in simple language.
From the standards, a clinical audit is designed which includes
- Objectives, stakeholders, patient inclusion/exclusion, and data collection period defined
- Data collection strategy outlined, and quality-of-care measures specified (including exceptions). Terms defined, data collection instructions provided
- Drafted by HQQ clinical audit experts, reviewed by the MoH Clinical Excellence Department and Saudi clinical expert groups
- Quality-of-care measures meet internationally published criteria.
Developing the data collection process
- Data collection protocol and criteria for the design of data collection forms.
- Process for developing the data collection forms
- Detailed instructions for data collectors
- Workshops for data collectors
To ensure the reliability of the data collected, clinical audits are conducted by multidisciplinary teams, workshops are conducted before and after data collection to provide ongoing support to hospital teams, and data are reliability checked.
Preparing hospital teams
- Hospital teams are multidisciplinary, focusing on aspects based on current evidence
- Workshops conducted before data collection for clinical care standards preparation, after to improve compliance
- Ongoing support for hospital teams
- Data validation workshop for independent validators ensure reliability, 85% agreement threshold, actual reliability was >95%
- Data “cleaning” and corrections requested
- Detailed before and after change reports were provided to everyone.
This systematic approach improves patient outcomes and delivers high-quality care.
Examples of the impact of pilot national clinical audits
Stroke patients:
- Increase in patients with ambulance alerts, NIHSS assessments, and swallow screens in 4 hours
- Increase in patients closely monitored for temperature, blood glucose, and receiving LMWH
MI patients:
- Increase in patients receiving fast and appropriate ED assessment and cardiac cath lab transfer
- Increase in patients referred to cardiac rehabilitation programs.
Major trauma patients:
- Increase in patients with trauma team leader present upon arrival
- Increase in patients with pain relief and rehabilitation plans.
Sepsis patients:
- Increase in patients receiving prescribed “bundle” of care on time.
Impact on patients and the public
- Improved clinical outcomes
- Improved patient-provider communication
- The assurance that clinical care in the MoH hospital is consistent
- Access to clinical care standards.
- More confidence in the care provided
Impact on clinical staff
- Credible clinical care standards
- Successful pilot national clinical audits, no challenges in 13 workshops with hospital staff
- Credible data collected through independent validation, no challenges to initial reports
- Hospitals willing to improve clinical practice, all submitted improvement plans
- Multidisciplinary team involvement driving cultural change
- Staff education and professional development prioritize meeting clinical care standards.
Impact on participating hospitals
- Hospital management aware of clinical effectiveness and patient outcomes gaps
- Direct feedback to clinicians on patient record-keeping quality
- Experience with applying quality improvement to effective care delivery
- Use of hospital information systems for standardized practice using pathways and protocols
- Sharing success stories of improved clinical effectiveness among hospitals.
Benefits of linking outcomes and clinical audits

Clinical audits are powerful in enhancing healthcare quality, benefiting patients, staff, and hospitals. Multidisciplinary teams, data validation, and evidence-based standards drive successful audits. The UK and the Middle East have reaped significant benefits, making clinical audits a valuable approach for all healthcare organizations to ensure high-quality care delivery.
FAQs
Q. What is the role of patients in a clinical audit?
A. Patients should have a voice in clinical audits. National Clinical Audits require patient representatives to have their say in what’s important to them from a patient care point of view. Local Clinical Audits can gather evidence from patients, and patient groups can collaborate and provide strong opinions and experiences from being patients.
Q. Are National Audits mandatory in the UK?
A. Of the 50 audits listed in the UK, about 25 of them are mandatory for National Health Service (NHS) organizations. If NHS organizations do not participate in these audits, they do not receive funding. Other audits that come from charities or professional groups are voluntary, but many groups participate anyway.
Q. Can clinical audits be done for a single hospital? What is the role of quality professionals?
A. Yes, clinical audits can be done at the local organizational level. Quality professional staff can be involved in clinical audits, but they need specialized training, particularly on what makes clinical audits unique and the importance of the discipline of data analysis.




