Adaptive Design: The Key Ingredient for successful large-scale improvement initiatives- Project Five life!
Read the Magazine in PDF
Abstract
The Ghana project reduced child mortality using quality improvement methodology. Scaling up gradually from districts to national coverage, involving teams, and partnering led to success. Effective strategies included establishing priorities, testing approaches on multiple sites, fostering idea exchange and resource sharing, and allocating sufficient infrastructure resources. A strategic, well-planned approach can achieve a significant impact and improve healthcare outcomes.
Introduction
The Institute for Healthcare Improvement has coined the term "pilot traders" to describe individuals who implement projects on a small scale and achieve positive outcomes but struggle to replicate those results at a more significant, national level.
Scale Up Design
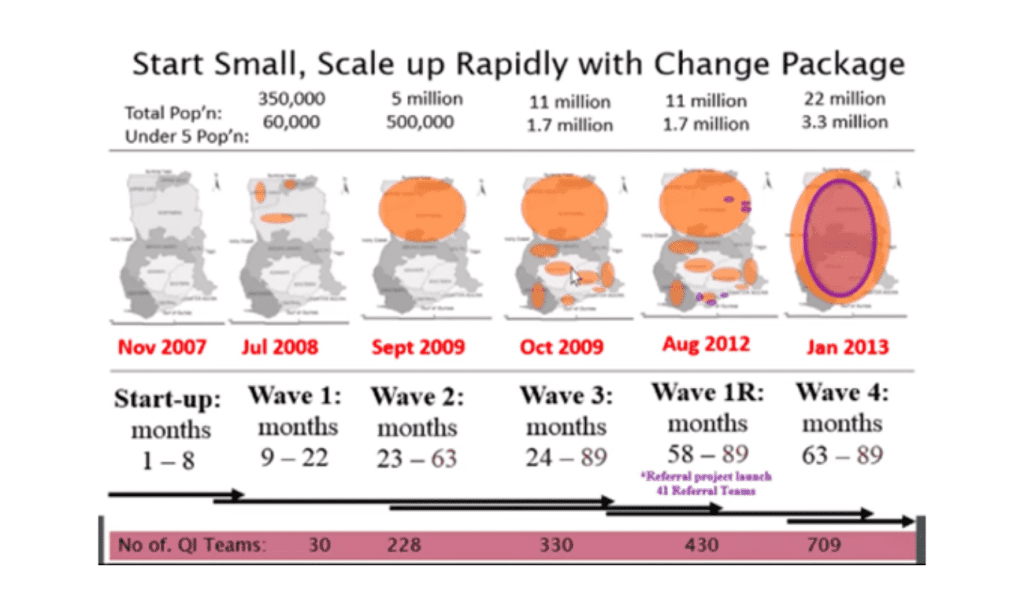
The Ghana initiative, funded by the Gates Foundation, aimed to reduce child mortality rates with quality improvement methods. Partnering with Catholic Health Service and Ghana Health Service, independent evaluation by the University of North Carolina ensured success. Starting with three districts, it rapidly expanded to cover 38 districts and numerous hospitals, eventually scaling up nationwide. The involvement of 709 quality improvement teams contributed to its success, reaching approximately 30% of districts and 80% of public hospitals in Ghana.
The IHI Scale-up framework
A scalar framework has been utilized for the implementation approach. In this framework,
- The first step is to establish priorities and align them accordingly.
- The second step involves designing a scalable unit, which can be a health center, a hospital, or an entire district.
- The third step is to structure the implementation process. Utilizing health system structures and learning from outcomes improves scalability. Testing in various settings and creating a platform for change appreciation enhances success and scalability. Leveraging evidence-based publications, frontline ideas, and available personnel contributes to initiative success.
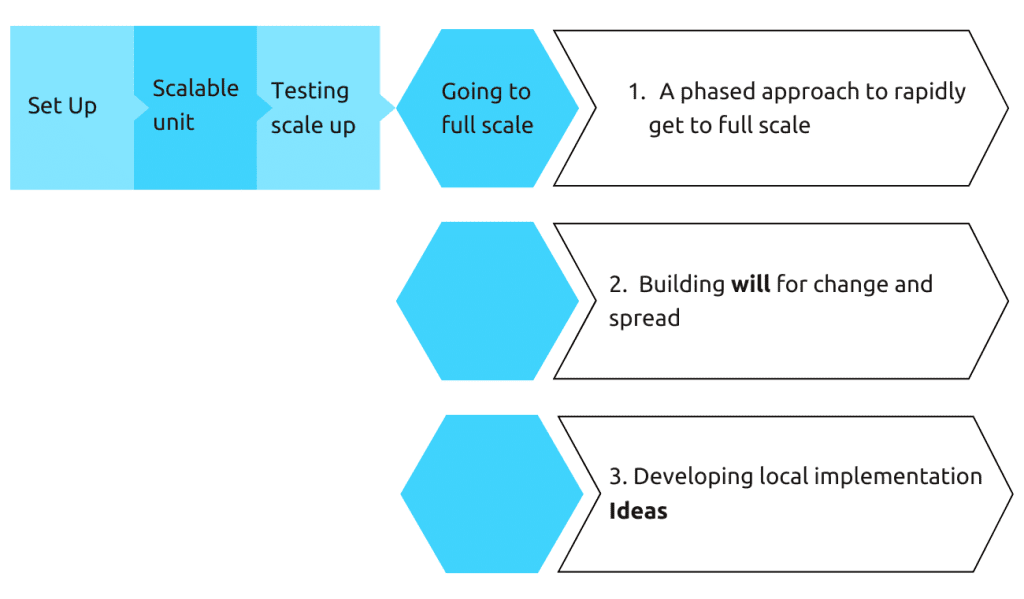
How do you build will?
Alignment is critical for success. When priorities match, like quality improvement and promoting data use in maternal and child health, success is more likely. Situating the methodology within the existing structure increases the chances of success.
Methodology and Strategy
The model for improvement is crucial, using process analysis to identify mortality causes and gaps. Quality improvement teams intervene to improve processes.
The model has three questions and a rapid cycle of improvement including:
- Setting ambitious aims
- Establishing a measurement framework
- Making specific changes to the test
- Implementing the changes on a larger scale
The model has three questions and a rapid cycle of improvement including:
- Setting ambitious aims
- Establishing a measurement framework
- Making specific changes to the test
- Implementing the changes on a larger scale
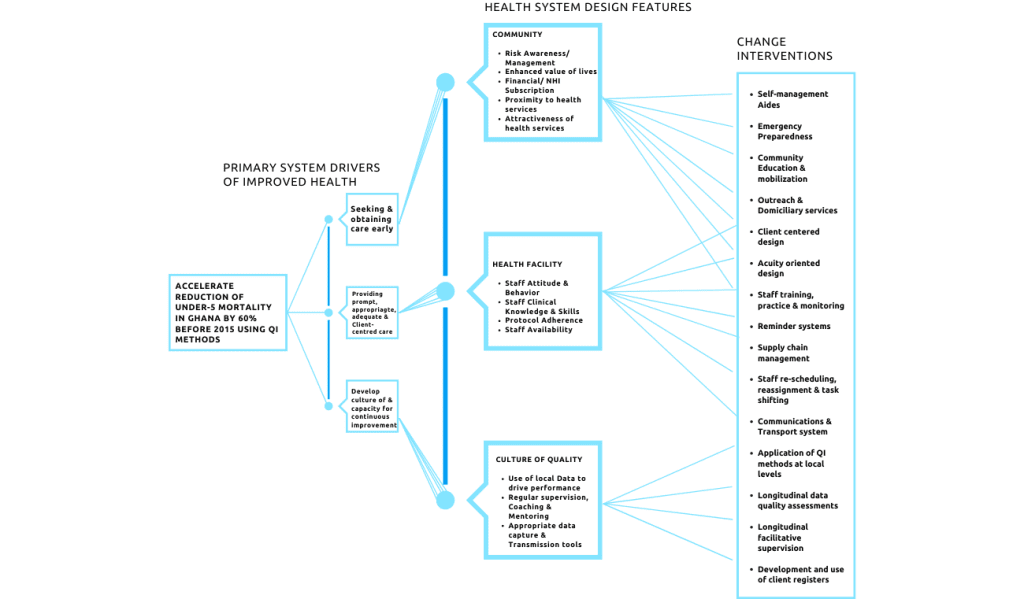
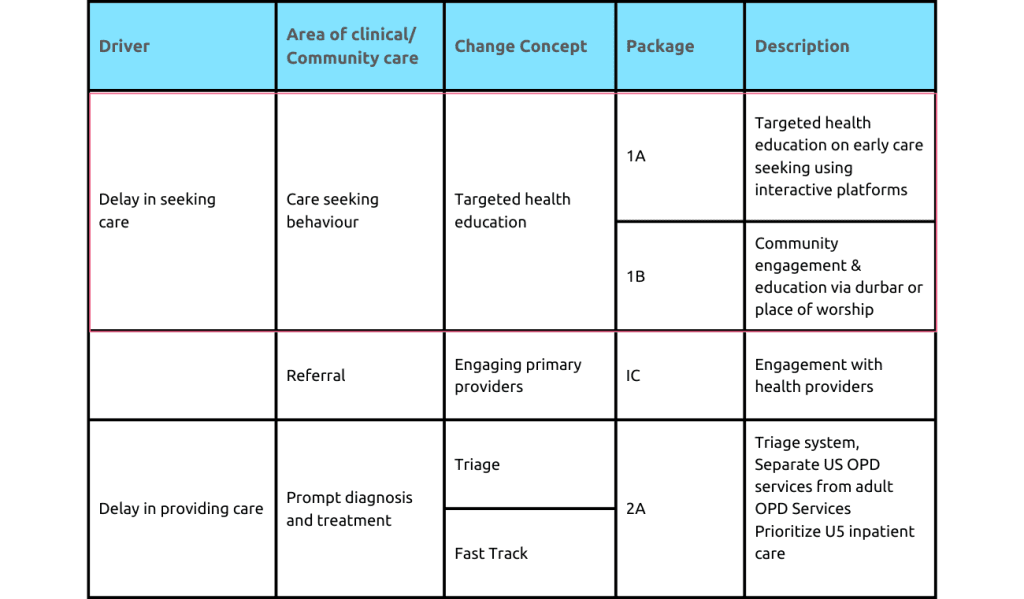
This theory of what is causing mortalities is captured in a driver diagram that focuses on the sub-district level, specifically on how to accelerate the reduction of mortality. The diagram has three primary drivers:
- Seeking early care
- Providing prompt care
- Promoting a culture of data use for improvement
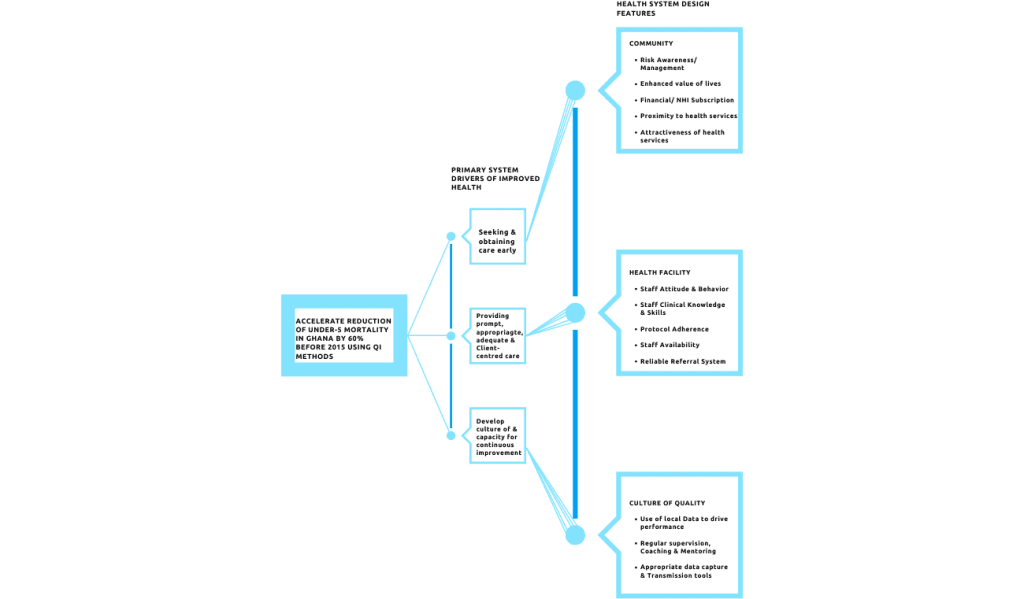
Teams identify key health system features impacting drivers, determining primary and secondary problems based on data. PDSA cycles implement and test interventions, gathering data for modifications. This systematic approach shows initiative effectiveness and efficiency.
But how can teams ensure that their initiatives are successful?
There are a few critical factors that must be considered:
- Clear goals: Establish clear goals with specific outcomes and timelines.
- Effective leadership: Leaders must be committed and willing to make changes.
- Data-driven decision-making: Use data to guide decisions and measure success.
- Collaboration: Work collaboratively within and outside of organizations.
- Rigorous testing: Test change interventions on a small scale and learn from the data
Small-scale testing of change interventions allows rigorous data collection. Once significant changes are demonstrated, they can be learned and adapted accordingly.
Strengthening community linkage
To enhance maternal and child health, the focus shifts to health facilities. Learning sessions include community health nurses, volunteers, and attendants to address gaps. Process maps identify decision points, like the husband’s consent or traditionalist involvement. Community engagement and changing teaching methods are vital. Solely training attendants is ineffective if women believe community-based deliveries are required based on husbands’ or traditionalists’ authority.
Innovative Changes
Community involvement revealed the need for changes in teaching methods. Visual aids, like pictures, were used to educate on anemia and birth preparedness. This saved transportation costs and improved condition management during labor at the right level of care.
When seen in the specialist clinic, individuals with long COVID should undergo a thorough assessment, including a review of their medical history and a physical examination. Initial management involves offering reassurance and support, with possible referral to specialty clinics if needed.
Healthcare professionals should coordinate care, stay updated on the latest evidence, and collaborate with patients to develop a tailored management plan.
Content Theory: U5 deaths in hospitals
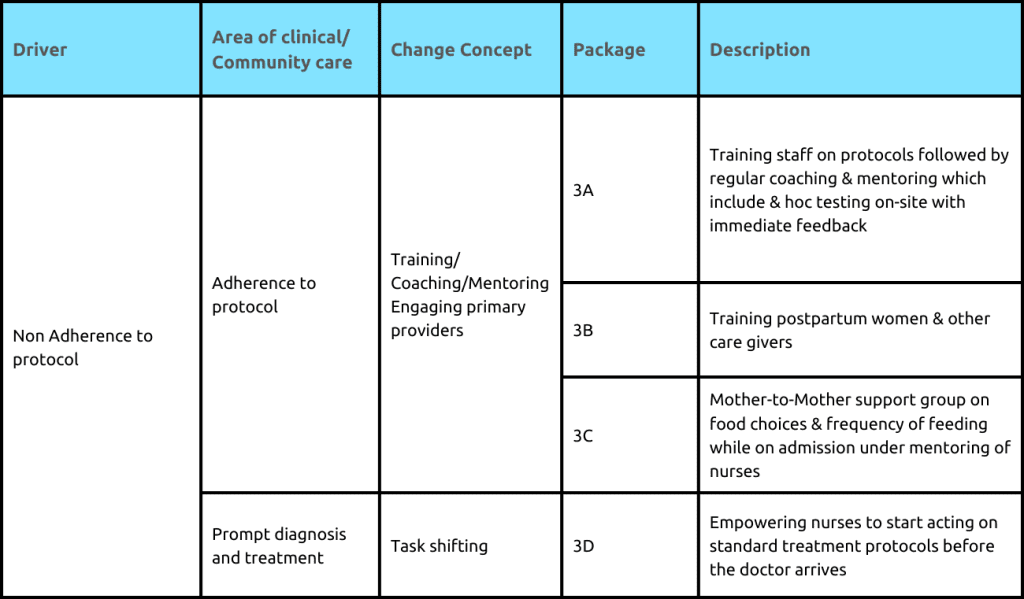
Initially community-level interventions, but later included hospital-level interventions. The three-delay model identified issues in early care-seeking and hospital protocols. Data analysis revealed malaria and respiratory infections as the main mortality causes. Secondary drivers and process measures were developed for hospital performance tracking. Delays in care and protocol adherence were critical to improving patient outcomes.
Making care processes more reliable
With training and interventions, a facility improved malaria treatment protocols. Initially, unreliable adherence led to high mortality. A data-driven approach achieved over 95% of children receiving evidence-based treatment, leading to significant outcome improvement.
Moving to the test of Scale
After successful community and facility interventions, the focus shifts to consolidating and documenting strategies’ success. A learning collaborative explores effective evidence-based implementation.
Specific successful interventions, like using ward rounds for teaching, are compiled into a “change package” for broader implementation in similar contexts.
Hospital Change Package
Change Package implementation reduced mortality rates in six of nine hospitals by 17% over 18 months. Challenges in management support affected some hospitals. Still, the project achieved a 35% reduction in under-five mortality and a 38% reduction in child malaria-related deaths, contributing to national maternal and child health improvements, and showcasing healthcare interventions’ potential impact
National Scale of the hospital change package
The Ghanaian project’s success in improving maternal and child health results from efficient management support, national quality policy, and sustainability focus. Cost-effectiveness and data quality reinforcement were prioritized. Lessons can inform other settings to improve outcomes, emphasizing investing in staff and systems. Strategic planning, strong leadership, and integration within healthcare systems are crucial for achieving lasting benefits. Adopting these practices can significantly impact maternal and child health initiatives.
Results
The project focused on skilled deliveries, increasing from 55% to 80%. Documenting changes is crucial for replication. Six prototype hospitals reduced mortality by 50%, contributing to a 17% reduction. Weak support, team dynamics, and attrition affected three hospitals. Accurate data reporting is vital for improvement efforts.
Nationally, impressive results: 35% under-five mortality decrease and 38% malaria-related deaths reduction. The project significantly contributed to these outcomes, reflected in the demographic health survey. The intervention was instrumental in achieving success.
Building Infrastructure for Scale
The next step is implementing the Prototype and scaling up interventions with established infrastructure. Challenges were addressed by the National Quality policy and strategy. Independent evaluation demonstrated the cost-effectiveness of training for long-term outcomes. Improving data quality relied on a protocol and Learning Network for data officers. Governments and health system managers should invest in staff for significant benefits.
Over 350 improvement coaches from Ghana Health Service play a crucial role in driving future efforts. The National Quality Policy outlines interventions at various levels. Discussions for incorporating quality improvement concepts into education and training are ongoing. The Ubora Institute, in collaboration with Ghana’s Ministry of Health, provides training and support in Ghana and other countries.
Lessons learned from the project are documented in “Lessons Learned from Ghana for Their Future,” a practical resource for similar initiatives.
Lessons learned
- Use a complementary approach: Combine Lean, Six Sigma, accreditation, and policy methods.
- Incorporate training in health professional curricula for skilled practitioners.
- Design interventions for sustainability and engage all health system levels from the start.
- Invest in improving data system quality and reliability.
- Layer interventions along existing health system structures for easier uptake.




