Patient Experience
Read the Magazine in PDF
Abstract
A Crohn’s patient shares her 20-year journey, diagnosed as a young adult. She uses the Spoon Theory to depict daily struggles with chronic illness, stressing patient-centered care. NHS England’s personalized care model supporting physical and mental health is discussed. The article offers tips for healthcare professionals on effective delivery.
A Brazilian dentist named Ms. Isabela Castro shares her transformative encounter with Matheu, a Meckel-Gruber Syndrome patient with an encephalocele, which prompted her shift to pediatric dentistry. The experience taught her the significance of patient care beyond textbooks. It inspired her to pioneer specialized sectors like special care dentistry, home care, hospital dentistry, and geriatric dentistry, driving change for a better patient experience.
Introduction
As a child, she enjoyed a healthy, carefree life, dreaming of becoming an actress or a barrister. At 16 or 17, she fulfilled her dream of traveling the world. However, her life took an unexpected turn when starting her career as a barrister at 19, she underwent surgery for what was initially thought to be a simple gynecological issue but turned out to be Crohn’s disease. Feeling frightened and judged, she struggled to get a proper diagnosis and was told it would be a mild inconvenience, only to realize it was far more challenging than she ever imagined.
Beginning of the speaker’s journey (Ms Anna Edwards)
Over the next two decades, she faced an uphill battle with Crohn’s disease, enduring numerous surgeries, pain, and various health complications. She felt unsupported by some healthcare professionals and experienced a wide range of negative emotions, including fear, insecurity, and feeling misinformed. To explain the challenges of living with a chronic illness, she turned to the Spoon Theory, which uses spoons as a metaphor for daily energy levels. People with chronic illnesses have fewer “spoons” to allocate throughout the day, making decisions about priorities crucial.
She was fortunate to have a good team of doctors, but not everyone is as fortunate. Understanding and support from others are essential for those with chronic illnesses. Each day brings varying levels of energy, and navigating life with a chronic condition requires constant adaptation. With empathy and awareness, we can better appreciate the struggles faced by those battling chronic illnesses and provide the support they need to live fulfilling lives despite their challenges.
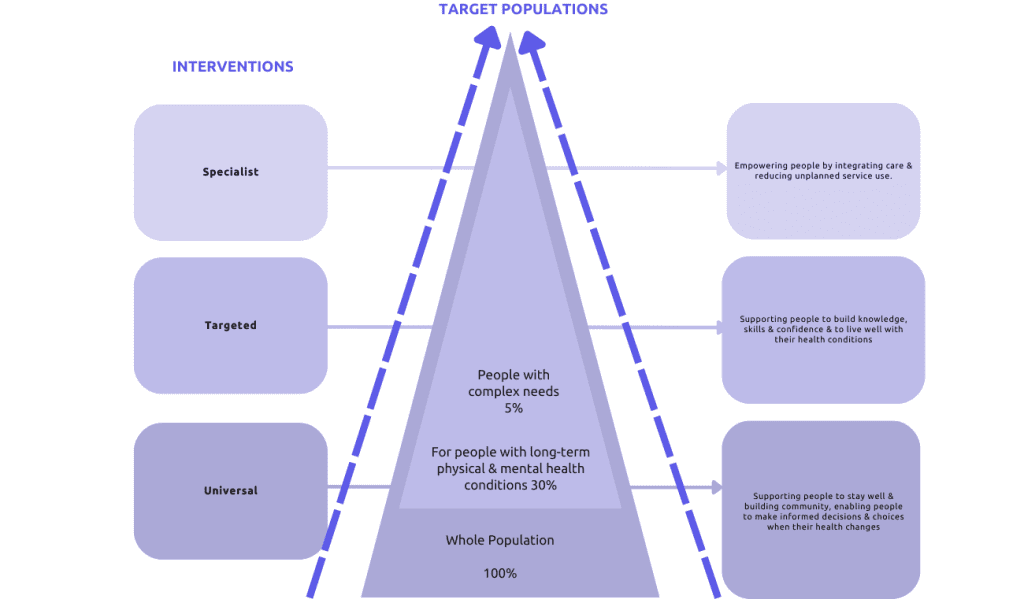
The NHS England model of personalized care aims to support individuals and caregivers in managing their physical and mental health while building community resilience and promoting informed decision-making about health.
It employs a whole population approach, offering specialist care, targeted care, and universal care to diverse population groups with varying health complexities. The ultimate goal is to empower people to lead healthy lives and make well-informed choices.
Comprehensive Personalized Care Model
All ages and whole populations approach to personalized care
As a health and social care professional with years of experience, she faces various barriers and facilitators to implementing patient-centered care. Time and resource constraints limit the extent of individualized attention each patient can receive. National payment and funding systems pose challenges, as do organizational processes and technology. Additionally, promoting a patient-centered approach may face resistance from leaders and a culture that does not readily embrace it. Patient receptiveness can also vary.
Evaluating the effectiveness of patient-centered care proves challenging due to the unique nature of each patient’s needs and presentations, making it difficult to gauge successful implementation.
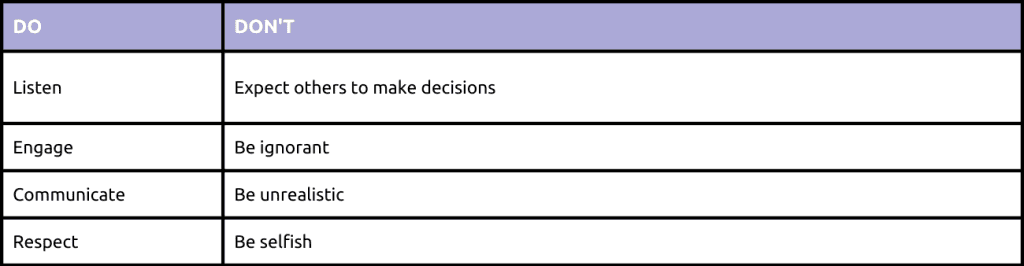
Effective person-centered care relies heavily on communication. Healthcare professionals should humbly inquire about patients’ priorities without assuming their needs or preferences. Trust is crucial, especially in virtual consultations and amidst pandemic-related fears and changed service access. The concept of “individualized empathy” resonates, recognizing the significance of each patient’s consultation and tailoring the approach accordingly. Listening attentively and understanding patient concerns without preempting personal opinions are vital aspects of person-centered care.
Encountering diverse patients with varying levels of engagement and articulacy, along with potential language barriers and mental health conditions, makes it challenging to tailor person-centered care to everyone’s needs. Patients themselves also play a role in the process. Overall individualized care that acknowledges and respects each patient’s uniqueness is essential for successful person-centered care implementation.
Patient participation is crucial in healthcare through active listening, engagement, and communication. Unrealistic expectations or self-centeredness can hinder this process. Involving patients’ families or advocates when needed is important. She aims to educate patients on self-advocacy to assert opinions confidently and be heard. Patient-centered care empowers individuals, ensuring they don’t feel isolated or unsupported.
Why patient care matters to the speaker? (Ms Isabela Castro)
Dentist Isabela Castro from Rio de Janeiro, Brazil, values patient experience as both a provider and a patient. A significant encounter transformed her perspective on healthcare systems, inspiring her to advocate for change. She believes storytelling can touch hearts and drive improvements in patient care beyond traditional learning.
Matheu’s Journey
She would like to share the story of Matheu, a patient whom she assisted while working as a dentist for the Brazilian Air Force during her early years. Matheu had a rare genetic condition called Meckel-Gruber Syndrome, which affects six different chromosomes and is characterized by occipital encephalocele, large polycystic kaidneys, and postaxial polydactyly. This syndrome is very rare, with an incidence ranging from 13,000 to 100,000, and can be diagnosed prenatally using ultrasound.
Matheu was born with a huge encephalocele in Brasilia, and his family already knew about his condition thanks to prenatal ultrasound.
However, after he was born, he was left in bed waiting for death because of the rarity of his condition. His father fought for his life and managed to get him transferred to Rio de Janeiro for surgical correction of the encephalocele.
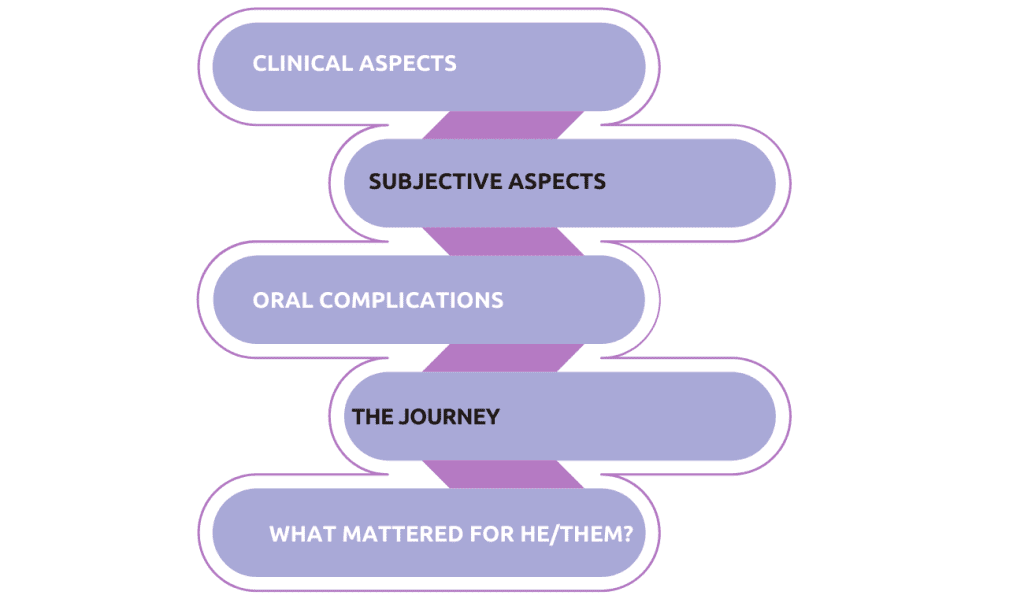
Matheu came to her hospital after the surgery and was in the neonatal intensive care unit. He had a tracheostomy, and a gastrostomy, and suffered from oral complications due to excessive bleeding. She was called to see him, and at that time, she was a freshman in the Air Force.
To go and see Matheu felt like a punishment. He had been suffering from pain and bleeding for days, and his mother was suffering watching it all happen. Matheu was a 22-month-old male patient with Michael Gruber syndrome who was admitted to the intensive care unit at the Air Force Central Hospital. He presented with Parker’s lips, extensive crusts, and a significant ulcer on the left lingual edge, measuring about two centimeters in diameter and covered with a pseudomembrane.
Over six months, the patient with Michael Gruber syndrome had an irregular ulcer, with frequent convulsions. Presumptive diagnosis: traumatic ulcer due to under-erupted teeth. Daily dental monitoring led to significant improvement, easing pain and bleeding. The experience taught me the importance of quality care as a right, and respecting patients and caregivers equally. Prioritizing what matters most, even breaking rules, can profoundly impact their lives. It’s not just another case for healthcare workers; it’s someone’s life.
When it comes to providing person-centered care, she often sees organizations – military, private, or public – claiming to prioritize the person, but upon closer inspection, the focus seems to be more on the disease and the physician.
As Ana mentioned, we need to empower patients and individuals to express what matters most to them and their caregivers, to improve their overall experience and journey. Just look at the satisfaction on this mother’s face after we connected and provided treatment.
As Ana mentioned, we need to empower patients and individuals to express what matters most to them and their caregivers, to improve their overall experience and journey. Just look at the satisfaction on this mother’s face after we connected and provided treatment.
Taking a closer look at what Matheu’s case has done for the speaker, Matheu has made her shift from a regular dentist to a pediatric dentist.
Upon reflection and thanks to Matheu, she realized that the healthcare system was not designed to prioritize those in need of better care. Rather, it dehumanizes patients. Despite her personal experiences with the disease, caring for her mother with depression, and her sister with cerebral palsy, nothing touched her as deeply as witnessing a suffering mother holding her son in the intensive care unit. This moved her to shift from her regular pediatric dentist and take a new perspective on the healthcare system. She decided to do what the healthcare system needs to do, and she realized that she had no idea of everything she have done. Matheu and his family were instrumental in transforming her and the system.
Matheus initiated a transformation in the healthcare system by establishing specialized sectors like special care dentistry, home care, hospital dentistry, and geriatric dentistry. His story inspired change, emphasizing that system outcomes should not be blamed on individuals but on the system itself. Patient transformation requires a system that allows communication between their needs and caregivers, ensuring a better experience.
The metaphor of the San Bernardino Bridge highlights the division between patients, caregivers, and the healthcare system. To improve healthcare, collaboration is essential, and the system needs to be rebuilt to prioritize patient-centered care. Working together, healthcare professionals, patients, and families can create a more effective and compassionate healthcare system.
Conclusion
The two personal stories of patients and healthcare providers highlight the importance of patient-centered care and personalized healthcare. Both stories illustrate how healthcare professionals can provide effective care by understanding the unique needs of each patient and tailoring their approach accordingly. The Spoon Theory, as explained by the patient with Crohn’s disease, serves as a powerful metaphor for the daily struggles of those with chronic illnesses, emphasizing the need for empathy and understanding from healthcare providers. The Brazilian dentist’s experience with Matheu illustrates how personal experiences can shape healthcare providers’ understanding of patient needs and lead to transformative change in healthcare systems.
Ultimately, these stories underscore the importance of prioritizing patient-centered care and personalized healthcare to improve the patient experience and achieve better health outcomes for all.
FAQ
Q.How would you encourage patients to speak up about their thoughts? What is the first step for that?
A. The first step is to educate patients about the role they can play in their healthcare. Patients can use available technology and resources such as Google to understand the things they should expect from healthcare. It is also important to empower patients, which can be achieved through doctors and healthcare professionals who create conversations that empower patients.
Q. Would you have any educational program for medical professionals doing so?
A. It is not that straightforward, as it requires a cultural shift across the world. However, there are educational programs for medical professionals on patient-centered care and patient empowerment.
Q. What is the difference between patient satisfaction and experience?
A. Patient satisfaction is related to the expectations a patient has about their healthcare journey, and it can vary depending on which part of the journey they are in. Patient experience, on the other hand, is related to every single touchpoint a patient has during their journey and goes beyond contact with the physician or nurse. It includes everything from noises to conversations in the corridors and more.
Authors
-

Head, Clinical Outcomes & PPE COVID-19 Task Force, Cabinet Office, Westminster, London
-




