Infection Control Risk Assessment
Read the Magazine in PDF
Abstract
The article highlights healthcare and patient safety topics, including Argentinean public health research, infection control, combating antimicrobial resistance, the built environment’s role in pathogen transmission, and challenges in Latin American healthcare. It stresses the need for comprehensive strategies to enhance care quality and presents successful collaborations and clinical trials. Despite high health spending, the region faces issues leading to inequity and increased COVID-19 mortality rates.
Introduction
IECS in Argentina focuses on improving healthcare globally, with projects on mother and child research, healthcare quality, patient safety, and health technology assessments. Collaborating with ISQua, efforts are made to enhance care quality worldwide. COVID-19 exposed weaknesses in health systems, emphasizing the need for improvement. Low-income countries face challenges of healthcare-associated infections and antimicrobial resistance, leading to higher mortality rates, emphasizing infection control and responsible antibiotic use.
Why care about infection control?
Infection control professionals have been vital in improving care for 40+ years, gaining recognition amid challenges from hospital-acquired infections and antimicrobial resistance. Preventative measures are crucial to tackle rising infection rates, minimize hospital stays, and reduce mortality, especially with increased risks of surgical site infections and limited antibiotic effectiveness.[1]
The 2016 paper stresses patient safety in 2030 as vital for healthcare quality, tackling preventable harm and economic burdens. Politicians recognize the impact of unsafe care on healthcare systems and resources, with patient safety and antimicrobial resistance on the G20 healthcare agenda, underscoring global significance. [2].
This report discusses four challenges facing patient safety.
- The first challenge is the increasing complexity of cases
- The second challenge is the constraint in budgets.
- The third challenge is antimicrobial resistance.
- Lastly, the report highlights the importance of patient safety for health systems

Various approaches to tackle antimicrobial resistance include research, antibiotic conservation, awareness raising, and surveillance. However, sanitation, hygiene, and infection control are crucial in combating the issue. ICRA’s involvement is essential in addressing hospital-acquired infections, which are prevalent in both low and high-income countries, exacerbated by the COVID-19 pandemic. Unprepared facilities contribute to the spread of multi-resistant germs, highlighting the need for improved hospital design and infection control measures. ICRA focuses on assessing healthcare providers’ readiness to deliver safe care. The 2013 paper stresses the significance of the built environment in pathogen transmission, emphasizing infection prevention during construction and healthcare facility design.[3]
1. Study Title: Role of Health Care Facility Design in HAIs. This 2012 study explores the impact of the built environment on healthcare-associated infections (HAIs), affecting 1 in 20 hospital patients in the US. Understanding the link between design components and HAI development is vital for effective infection control measures and patient safety. The study includes a conceptual model, a comprehensive literature review, and interviews with professionals in infection control, air and water quality, hospital management, design, and architecture. It sheds light on addressing HAIs through environmental considerations.

The framework emphasizes hospital reservoirs as germ sources, requiring hygiene measures to prevent patient colonization. It highlights the crucial role of contamination elimination during construction to reduce hospital-acquired infections.
ICRA is a multidisciplinary process that coordinates knowledge to anticipate impacts and lower infection risks in healthcare facilities.
ICRA Phases:
- Design: Long-range planning considers isolation rooms, ventilation, filtration, and addressing contaminated water systems like Legionella.
- Construction: Identify hazards, relocate vulnerable patients, deploy barriers, and protect HVAC and water systems.
- Mitigation: Consider patient placement, standard barriers, temporary provisions, and protection during demolition to prevent contamination.
ICRA is critical in preventing healthcare-associated infections. Awareness of potential risks is vital during healthcare facility planning, building, and maintenance. [4]
It is crucial to assess the nature of construction work, including the risk of dust generation and aerosolization of bacteria during activities such as demolition or drilling.
To identify the appropriate type of construction, there are four categories to consider.
- Type A involves inspection and non-invasive activities
- Type B refers to small-scale, short-duration activities that create minimal dust.
- Type C generates a moderate to high level of dust or requires the demolition or removal of fixed building components.
- Type D is the most invasive type, requiring major demolition and construction projects.
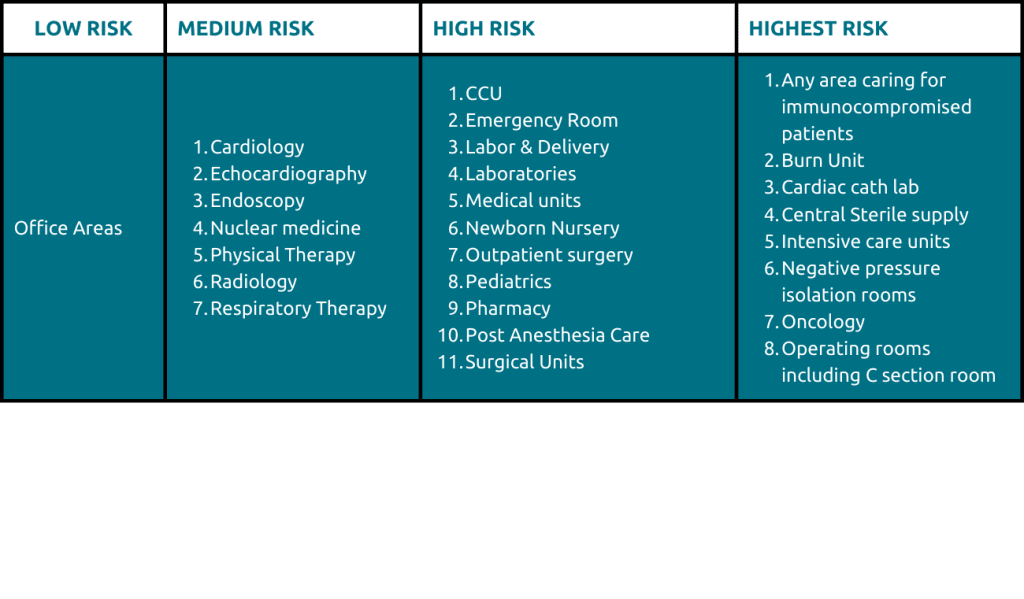
When planning nursing unit construction, consider areas like hallways, patient rooms, nurse’s stations, and patient care variations. The table links construction types with hospital areas, providing infection control recommendations. ICRA is crucial for patient safety during asbestos-related renovations. Regulatory oversight and record-keeping protocols prevent construction harm. Latin America’s healthcare investment varies, with waste and inequity issues.
When planning nursing unit construction, consider areas like hallways, patient rooms, nurse’s stations, and patient care variations. The table links construction types with hospital areas, providing infection control recommendations. ICRA is crucial for patient safety during asbestos-related renovations. Regulatory oversight and record-keeping protocols prevent construction harm. Latin America’s healthcare investment varies, with waste and inequity issues.
The Latin American Consortium for Quality, Patient Safety, and Innovation (CLICSS) advocates implementing specific recommendations and prioritizing actions to enhance healthcare quality and patient safety in the region.[5]
The Latin American Consortium for Quality, Patient Safety, and Innovation (CLICSS) advocates implementing specific recommendations and prioritizing actions to enhance healthcare quality and patient safety in the region.[5]
A local network prioritizes care quality and patient safety, issuing a pandemic call to action. They urge integrating policies for vulnerable populations, reorganizing patient flow, strengthening supply chains, and promoting self-protection among healthcare providers. Person-centered care and effective communication are emphasized. Publications serve as infection control examples. In Latin America, collaboration reduced CLABSI frequency in ICUs, offering lessons for the Indian subcontinent. Scaling up interventions through collaboration effectively addresses CLABSI and improves care in the region.
The collaborative project ‘Adiós Bacteriemias’ successfully reduced CLABSI incidence by 56% in 39 Latin American ICUs through care bundle implementation. In the second phase, 83 ICUs from five countries achieved a 22% reduction in CLABSI incidence rate. The BTS Collaborative model guided implementation through virtual learning sessions, improving compliance with CL insertion and maintenance practices. Noncompliance with standardized health procedures contributes to higher CLABSI incidence in Latin America compared to the United States.[6]

In Argentina, a clinical trial is underway to enhance HAI rates through evidence-based interventions, specifically targeting hygiene in ICUs. This study contributes to the existing knowledge on HAI and proposes a scalable solution for improving ICU hygiene. This example demonstrates the effectiveness of multi-dimensional interventions in addressing HAI issues, particularly in transitional countries like Argentina.
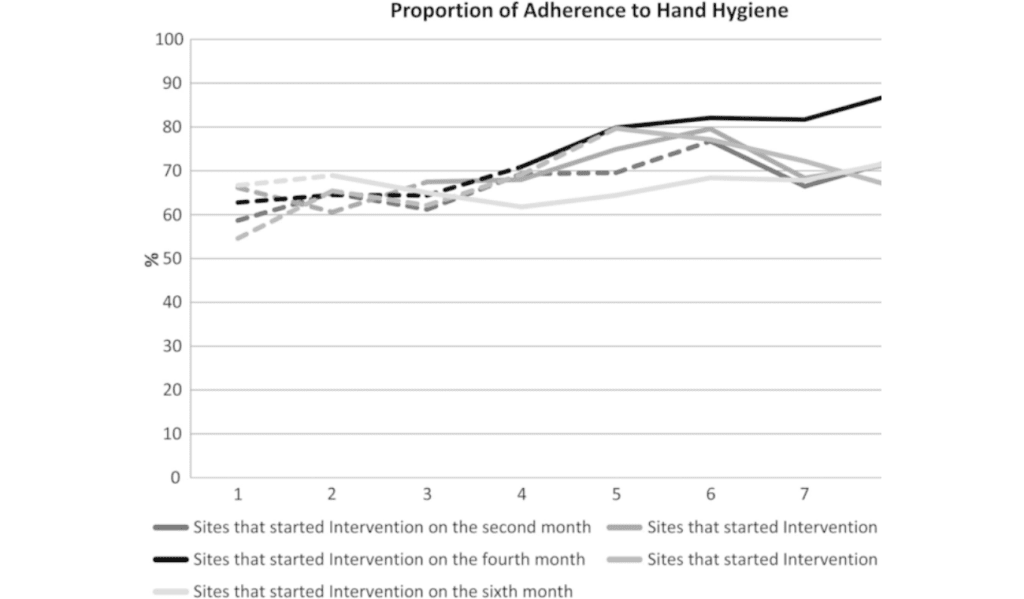
A cluster-stepped wedge trial in 11 ICUs in Buenos Aires implemented a multimodal intervention for hand hygiene improvement. The approach included leadership commitment, surveillance, reminders, a storyboard, and feedback. Involving 705 participants, the intervention group achieved significantly higher compliance (75.6%) compared to the control group (66.0%). The intervention remained effective even after adjusting for calendar time and provider characteristics. This study demonstrates the effectiveness of a low-cost, evidence-based multimodal approach in promoting and sustaining hand hygiene compliance among healthcare workers in ICUs.[7]
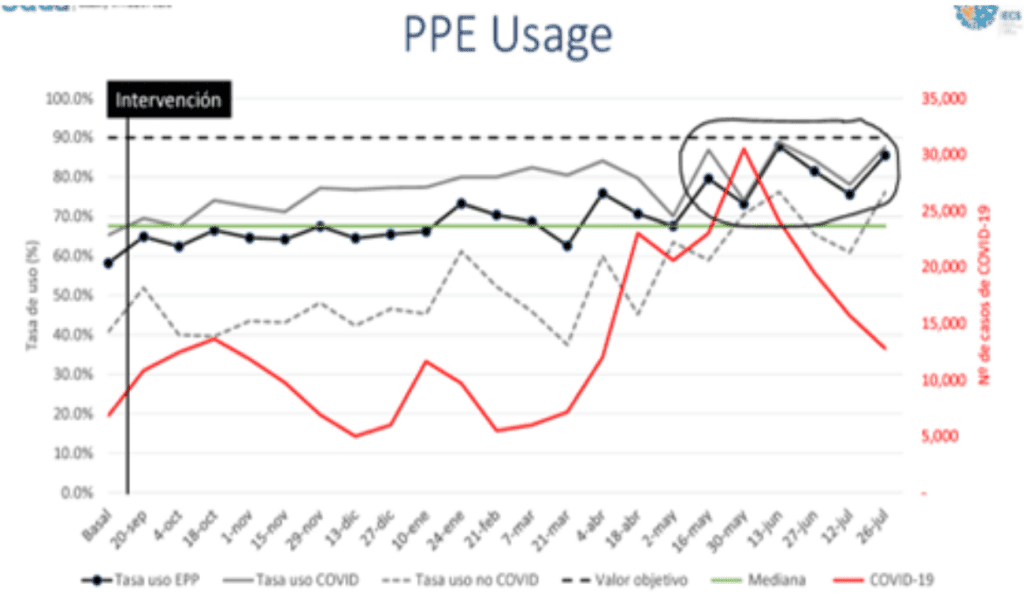
During the pandemic in Argentina, two infection control projects aimed to improve ICU outcomes. The first involved 15 ICUs, focusing on PPE usage, patient flow, bed shortages, and emotional support. The ongoing second project targets patient safety indicators using a collaborative approach over 56 weeks. Positive results were achieved, seen in the progress graph from September to July, despite a team member loss. PPE usage improved to nearly 99%, impacting contagion for providers and patients. A daily goals checklist addressed hygiene issues, leading to sustained improvement. Efforts are ongoing to address emotional support for healthcare workers. Antibiotic stewardship is crucial to combat increasing resistance. Collaborative efforts in ICUs play a vital role, especially in developing countries facing hospital-acquired infection threats. ICRA and quality improvement initiatives enhance patient outcomes globally.

Conclusion
Infection control is vital in preventing hospital-acquired infections and combating antimicrobial resistance. ICRA addresses hospital infections and the role of the built environment in pathogen transmission. Collaborative efforts are essential to improving healthcare in Latin America, addressing challenges like waste and fragmentation. Progress has been made in reducing CLABSI and improving hygiene rates. Incorporating quality and safety policies is crucial, especially for vulnerable populations. The interrupted and controlled time series project in Argentina during the pandemic showed positive results, emphasizing the need to sustain and expand efforts for equitable and safe healthcare in Latin America.
References
- Pacific, W., & Hasan, S. A. W. Patient Safety.
- NIHR North West London Patient Safety Research Collaboration.
- Premier Solutions. https://premierinc.com/solutions
- Arrieta J, Orrego C, Macchiavello D, Mora N, Delgado P, Giuffré C, García Elorrio E, Rodriguez V. ‘Adiós Bacteriemias’: a multi-country quality improvement collaborative project to reduce the incidence of CLABSI in Latin American ICUs. Int J Qual Health Care. 2019 Nov 30;31(9):704-711. doi: 10.1093/intqhc/mzz051. PMID: 31198929.
- Arrieta, J., Orrego, C., Macchiavello, D., Mora, N., Delgado, P., Giuffré, C., … & Rodriguez, V. (2019). ” Adiós Bacteriemias”: a multi-country quality improvement collaborative project to reduce the incidence of CLABSI in Latin American ICUs.
- Rodriguez, V., Giuffre, C., Villa, S., Almada, G., Prasopa-Plaizier, N., Gogna, M., … & Vidal, A. (2015). A multimodal intervention to improve hand hygiene in ICUs in Buenos Aires, Argentina: a stepped wedge trial. International Journal for Quality in Health Care, 27(5), 405-411.
FAQ
Q. Where does infection control start in hospitals?
A. Infection control begins with leadership support, enabling measures like ICRA and surveillance.
Q. What’s the main cause of hospital infections as per the speaker?
A. The lack of leadership backing for infection control is the core cause.
Q. How does the speaker view medical device reuse?
A. Generally opposes unsafe reuse, and supports regulated remanufacturing.
Q. How many infections could redesign prevent, according to the speaker?
A. The exact number is unknown; any preventable infection justifies proper redesign, highlighting infection control’s value.
Author
-

President-elect-ISQua; Professor Public Health, School of Medicine, CEMIC; Director-Admin and Dept of Health care quality and patient safety, IECS, Bueno Aires, Argentina



