Bridging the Gap: Addressing Cultural and Psychological Safety in Oncology Centers
Read the Magazine in PDF
Abstract:
Organization Profile:
In Qatar, the Ministry of Public Health oversees a well-developed healthcare system that offers services through two leading organizations: the Primary Health Care Corporation and the Hamad Medical Corporation (HMC). The HMC is the primary provider of secondary and tertiary healthcare and manages 12 hospitals, the National Ambulance Service and home and residential care services. The National Cancer Care and Research Center (NCCCR), established in 2004, is Qatar’s sole cancer care provider.
Introduction:
The State of Qatar, situated on the Qatar Peninsula, has a population of 90% expatriates from 94 countries. The Hamad Medical Corporation (HMC) manages 12 hospitals, including the National Cancer Care and Research Centre (NCCCR), the only cancer care provider in the country. In 2021, the NCCCR served patients from over 60 nationalities, with a staff of 30 nationalities. A review of the quality indicators of cancer hospitals was undertaken to meet the needs of a culturally diverse patient population, advancing technology and increasing patient expectations. The study aimed to put person-centeredness at the forefront, creating six new indicators, including the Net Promoter Score (NPS) and the existing two indicators.
Furthermore, creating a culturally and psychologically safe environment is crucial to ensuring the well-being of patients and is a fundamental right for every patient. However, due to the diverse cultural environment in which hospitals operate, gaps have been identified, and care providers must take extraordinary measures to address these gaps and mitigate potential risks to patient well-being.
The steps taken for the diagnosis of the problem were:
- The department reviewed its quality indicators to ensure continuous quality improvement.
- The review was based on the BC Health Quality Matrix, which considers advances in treatment techniques, the adoption of state-of-the-art technology, and the cultural diversity of staff and patients.
- The review focused on patient safety, clinical outcomes, and service excellence, with a patient-centric approach at every touchpoint.
- Eight relevant indicators were identified based on the quality dimensions mentioned in the BC Health Quality Matrix.
- One of the indicators identified was the Net Promoter Score (NPS) of the department, which reflects the dimensions of respect, safety, and equity.
- The department introduced a bilingual feedback form that collected Patient Reported Experience Measures (PREM) at various touchpoints to gather patient feedback.
- The feedback form also included information on violating patient rights, outstanding staff, and free text for comments.
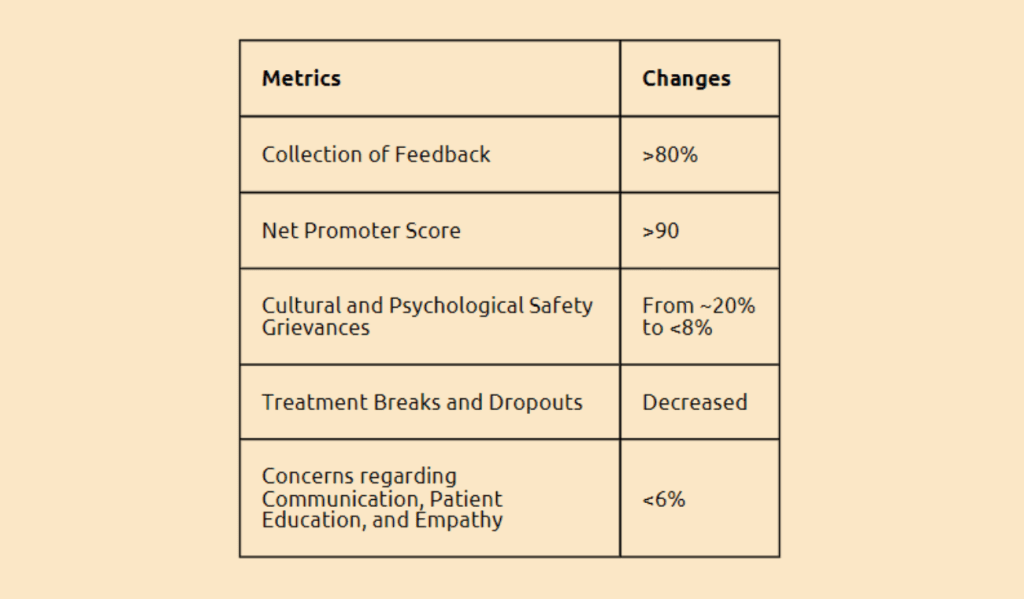
- Over the last year, the average feedback score was 81%, and almost 20% of the negative remarks were related to cultural and psychological safety concerns.
- Previously, these concerns had gone unnoticed or were diluted in the centralized feedback system.
- By implementing a department-specific feedback form and receiving feedback from over 80% of patients, the department was able to capture these concerns and address them.
- Root Cause Analysis of the patient grievances revealed that care providers must focus on effective communication to understand patient-specific requirements, enhance cultural sensitivity among team members, and become more empathetic in addressing patients’ needs.
Outcome:
A solution was found using the following methods:
- A lack of cultural sensitivity can be attributed to cultural awareness and competence. Initiating training programs and sharing patient stories are effective ways to create cultural awareness, sensitivity, and competence.
- Active involvement of team members, sensitizing pieces of training, and brainstorming sessions are used to gain the team’s confidence and modify the process flow based on patient feedback and RCAs.
- Voice of Customer (VoC) and patient-centric staff awards were introduced to motivate the staff.
- The staff onboarding program was strengthened by introducing a buddy system for new staff.
- NPS and PREM are efficient tools for understanding the service standards of the department and patient experiences against expectations.
- Department-specific PREM helps to understand cultural and psychological concerns.
- A proactive approach was introduced by asking patients and their relatives about specific requirements or concerns, so the team can address them.
- Clinicians communicate any specific requirements patients request to the rest of the team.
The following steps were taken to lock in the improvement:
- The report and Quality Indicator dashboards are shared with the entire team, along with pictures of the staff nominated for the most patient feedback.
- The Voice of the Customer and Patient-Centered Staff Awards are distributed annually during the Department Day celebration in November.
To replicate the improvement, the following steps were taken:
- Implementing the project at the Radiation Oncology department in NCCCR was successful.
- The discussion is ongoing to extend the project to other units of NCCCR, including the Daycare chemotherapy unit, Surgical unit, and IP units, to improve patient experience and standardize operational practices across the hospital.
Cancer Journey Mapping is in its conceptual phase in the State of Qatar

Conclusion:
The NCCCR in Qatar took significant steps towards improving patient experiences by redefining quality indicators, implementing a department-specific feedback form, and addressing cultural and psychological safety concerns through training programs and proactive approaches. By collecting and analyzing feedback and taking a patient-centric approach, the NCCCR was able to decrease grievances and concerns regarding communication, patient education, and empathy. The successful implementation of the project in the Radiation Oncology department and the ongoing discussions to extend the project to other units show the potential for this approach to improve patient experiences and standardize operational practices across the hospital.