Clinical communication in challenging situations
Read as Magazine PDF
”Person-centred, registry-enabled learning health systems can successfully co-produce better health, value and science by leveraging conversations and data.”
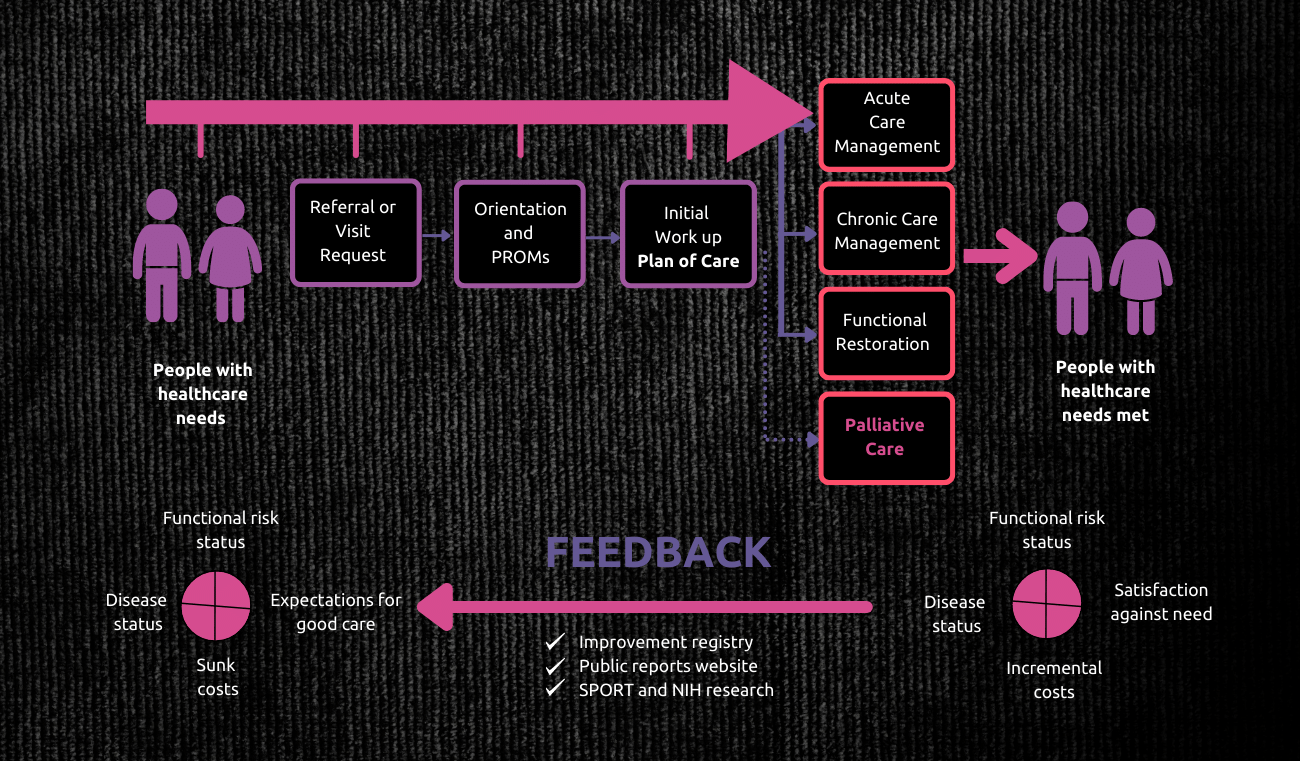
isa Weiss and Jim Weinstein, co-founders of the Dartmouth Spine Center, in the year 1998 started a new system for providing comprehensive spine care with a new information environment that supported better conversations and better decisions. A patient visiting is asked to complete a health assessment - that shows how they are doing and what their expectations of good care are. The summary information is shared with every patient - using them for better conversations to focus on outcomes achieved vs outcomes wanted. It is fed forward to the clinician and then it is used for a more sharp conversation about how the person is doing, choices and what to do next.
A dashboard is made from the health assessment. It takes about 20 minutes to summarise:
- Personal summary, work disability, health history, health habits, review of systems, history of present illness, red flags, clinical protocols, patient-reported health and wellbeing scores and indicating the present clinical status and tracking its progression in time.
- A tracker separately tracks the outcomes and compares them with the expectation.
Such data is further consolidated into various forms of analysis and assessments such as:
- Value Compass – to compare how the outcomes changed with various treatment models. This is usually compared to the parameters of clinical outcomes, functional outcomes, satisfaction and costs.
This information is fed back into the centres for real-time care. This allows for personalised risk calculators that allow me to take personalised informed decisions. This is the beginning of personalised predictive medicine − skating to where the puck is going to be. This system has resulted in over 100 publications and the work continues today.
In 2000, Steffan Lindblad was inspired by our work and he laid the foundations of the Swedish Rheumatology Quality Register. He summarised his view of our discussion as an equilateral triangle with patient, physician and partnership on the corners, all interconnected through communication. It is all about the partnership that is fuelled by communication.
This is presently implemented for rheumatology management across patients in Sweden. Every patient is given a health assessment, and they quickly learn how to read their dashboards. This shows the dates of visits tracked with patient-reported outcomes and clinical outcomes and is combined and highlighted and coloured and medications are also tracked.
In the diagram above, the patient had gone from borderline flare-ups to an all-out exacerbation of their arthritis from August to December. When their medication was changed at the end of November, the person returned to the resting disease state.
On a systemic level, this caused a cut in half of the disease activity rate of all the Rheumatoid Arthritis cases across Sweden in nine years. One of the counties (Gavle) that implemented the system considerably reduced its outcome variability and it immediately fell in line with and better than the national numbers.
Concepts: Developing a Conceptual Model
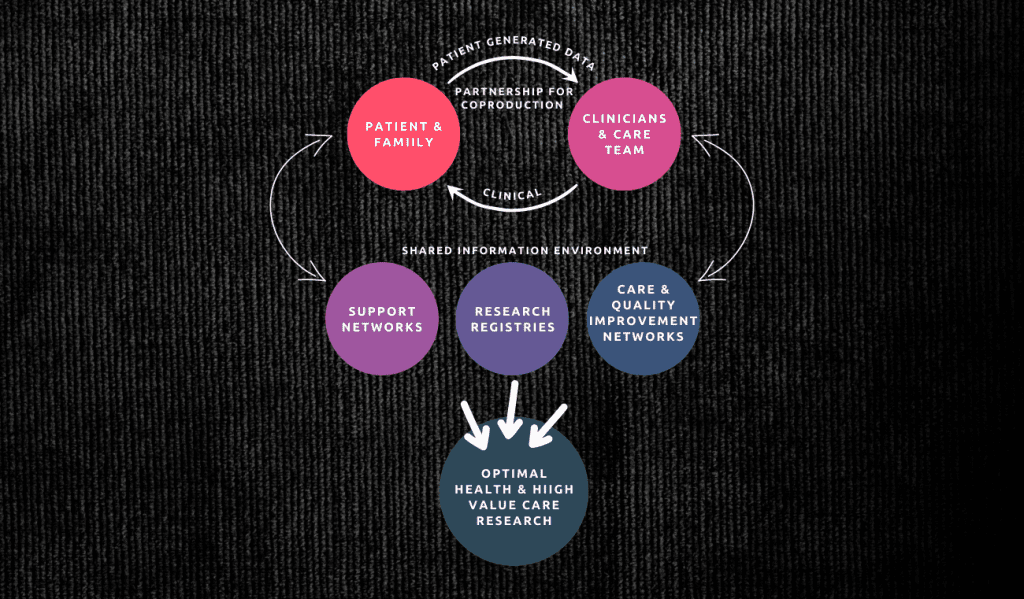
In October 2013, we met 10 people from Sweden who were instrumental in the implementation of the model. We drew up a model to summarise our brainstorming and we came up with two key areas: Social System Innovations, including Patient/Family Networks and QI/Research Networks, and Technological Innovations, including registries, HIT-enabled networks and Feedforward Feedback Data Flows under the label, Patient-Centred Decision Support for the Co-Production of Good Care and Better Health Outcomes.
The core of the model:
- Co-assess: Co-assess the patient’s health status and how the treatment plan has been working to improve the patient’s health and well-being.
- Co-decide: Co-decide on what the next steps in the patient’s treatment plan should be based on relevant evidence and past experiences to minimise the burden of disease.
- Co-design: Co-design the treatment plan for daily care and professional interventions to attempt to minimise the burden of treatment.
- Co-deliver: Co-deliver the treatment plan that usually involves daily self-management and adherence to the plan and occasional treatments by a professional clinician or clinical team.

”Person-centred, registry-enabled learning health systems can successfully co-produce better health, value and science by leveraging conversations and data.” - Wayne Gretzky, Former Professional Ice Hockey player
In healthcare, we need the same principle, to think ahead of time, to be ready for the changes before they happen.
Together, we bring the full power of our collective expertise to provide the best possible care to our patients, our people and our communities.
This model is currently being adopted in the treatment of various conditions, including:
- Cystic fibrosis
- Adult Crohn’s Disease
- Peds and rheumatology
- Palliative care/serious illness
- Cancer
- Kidney disease
- Multiple sclerosis
Core Concepts
Coproduction Defined: The independent work of patients and professionals to design, deliver, assess and improve the relationships and actions that contribute to the health of individuals and populations through mutual respect and partnership that leverages each participant’s unique assets, expertise and actions.
Learning Systems Defined (Senge): “Learning organisations are those organisations where people continually expand their capacity to create the results they truly desire, where new and expansive patterns of thinking are nurtured, where collective aspiration is set free, and where people are continually learning to see the whole together.”
Real-world examples of the success of the concept:
- Cardiac Surgery – Northern New England Cardiovascular Study Group — In eight years (1987-1995), the mortality was reduced from 4.5% to 3.5%. This continued until 2003, bringing the number to ~2%.
- Cystic Fibrosis – CFF Registry Enabled Learning Health System – Ten-year gain in life expectancy from 1990 to 2012 before breakthrough protein modulators were developed.
- Rheumatoid Arthritis – Swedish Rheumatology Quality Register – The mean inflammatory marker level has fallen from 12.6 to 3.12 between the years 2002 and 2017.
Serious Illness Conversation
The Serious Conversation Guide by Ariadne Labs is a framework to make conversations about seriously ill patients’ priorities more efficient, higher quality and more meaningful. It includes the following phases:
- Setup and introduction
- Assessment of the patient’s understanding
- Sharing the information about uncertainties, time, function and best and worst-case scenarios.
- Exploring the patient’s objectives and thought process
- Emphasising the most relevant points
The SIC Model of Care aims to systematically increase conversations between oncology teams and seriously ill patients to understand their goals before complications arise while making conversations more efficient, higher quality and more rewarding.
Integrating it with the MR makes it accessible at every successive stage. Having the conversation early allows the patient to process it better. Including perspectives of multiple experts from varying fields from practitioners to social workers and relatives of patients allowed for the development of a system that takes into account all considerations, allowing it to be much more readily accepted.
We included everyone in the training and developed one-to-one training for key personnel as a feedback mechanism for the work that they had just completed, allowing them to gain confidence and learn through practice.
We co-designed our eligibility criteria, and identified our barriers, our key drivers, our workflows and changed ideas.
Use of the SICG in oncology and high-risk primary care settings led to:
- Earlier discussions before EOL
- Increased EOL discussions before death
- Higher quality discussions followed best practices
- Documentation highly visible in MR
89% of clinicians using a guide elicited patients’ goals and values as against only 44% of the control group. (Paladino J, JAMA Oncol. 2019;5:801-809)
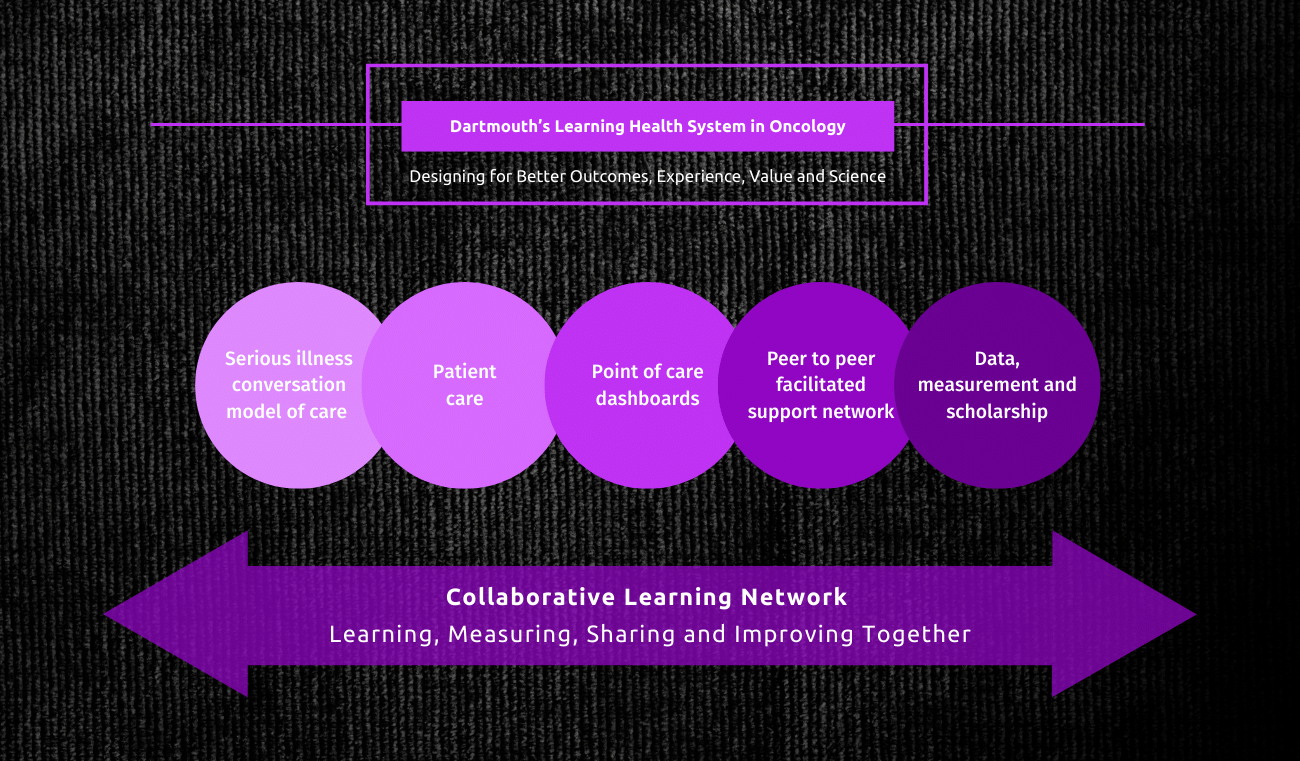
Patient anxiety was lower while following the process and the benefits lasted over 24 weeks. (Bernacki R, JAMA Intern Med. 2019;179(6);751-759)
The median time for the conversation was also reduced, increasing clinician efficiency with the nurses requiring about 26 minutes and physicians requiring about 22 minutes. 19% of conversations were completed by nurses and 37% were completed by physicians. (Lakin JR, Health Aff, 2017)
Implementation stages we went through:
- Development (five months): SIC Team formed, weekly huddles initiated, patient eligibility defined, provider training defined, workflow mapping completed.
- Kickoff (two months): Initiated SIC coaching and data sharing with the team
- Standard work (two months): Patient report out defined, scheduling script introduced based on VOC.
- Resources (two months): SIC completion, timing defined, expanded workforce capacity expansion
Introducing a scheduling script, incorporating the feedback of the patients in scheduling and other steps elevated our median percentage of eligible patients given the procedural conversation significantly. A pre-visit menu allowed patients to set their agendas and this makes the patients very confident in knowing what to ask and they can do that at a time that is suitable for them.
Benefits:
1. The PFA reduced clinicians’ barriers to initiating conversation.
2. Early conversations improved clinicians’ experience of delivering care
3. The LHS reframed clinicians’ perspective on their role in providing care
4. The LHS created team equity, a growth mindset and engagement
Conclusions:
1. Co-production learning health systems can improve health, healthcare value and science.
2. A key to their success is better conversations that forge better patient/physician relationships that focus on the patient’s goals and on treatment plans that have the best chance of achieving the outcomes that matter most to patients.
Authors
-

Prof. Community & Family Medicine The Dartmouth Institute for Health Policy and Clinical Practice
-

Assistant Professor, Medicine, The Dartmouth Institute for Health Policy and Clinical Practice



