Patient experience – by Anna Edwards
Read as Magazine PDF
We must acknowledge that while healthcare quality as a concept is universal, the road that leads to quality must be dependent on the context. - Dr Carsten Engel
MS. ANNA EDWARDS
MY STORY:
I was probably about six or seven. As a child, I had no problems. I was very healthy and happy. Very rarely attended the doctor. My parents can’t remember me ever attending the doctor’s surgery. So a very happy childhood throughout my kind of early years. I, like many others, have thoughts about what I’d like to do with my career. Initially, I wanted to be an actress, but my mother said that was not an appropriate career path. And so I suggested perhaps the barrister might be better, which she was much happier about. But one thing I wanted to do when I was about 16 or 17 was quite clear. I wanted to travel the world. I’m very lucky I’ve been able to do that. However, as I started my career as a barrister, I went off to university at the University of Manchester, which you can see there on the left. But a few weeks in I ended up in hospital having surgery for a baffling abscess, and it was considered at that point that this was just a straightforward gynaecological problem that would be easily solved, that it was urgent, and that it took some weeks to diagnose me with Crohn’s disease. At that time as a patient and I was 19 years old, I was pretty frightened. I felt a little bit judged because I had originally been admitted for a gynaecological issue. I felt very undermined. I felt like I had no real voice. I had no diagnosis for some time. And then when I did get a diagnosis, I was told it would be a mild inconvenience. So I remember those two words place a mild inconvenience. It felt very much top right-hand corner like the doctor was kind of thinking about what was wrong with me. I was doing lots of tests and things, but I was kind of thinking, What does this mean for me? Who am I? Who am I going to be? What does it mean for my career? What does it mean for my relationships with people? Is it going to have an impact? Me and my family and my ability to have a family. Is it going to kill me? I just didn’t know anything about it. And it was 20 years ago now, so people didn’t know what Crohn’s disease was then. So it was all rather overwhelming. And I was 19 years old, a young woman, just really starting in life. So I guess for the next 20 years or so, I felt like this. I felt like I was in a boxing ring. I was determined to fight this illness, whatever it was. But to be honest, I was going to get knocked down time and time again. I felt like I needed people on my side, people in my corner. And that not only were my family and friends, but also the health care professionals treating me. Why did I feel like this? Because this is what I had ahead of me. I have now had over 30 major surgeries. I’ve had an awful lot of pain. I’ve had temporary stigmas and permanent status. I now have a permanent one. I’ve had sepsis more than once. I’ve had pneumonia. Both my kidneys failed. At one point, after IVF infertility surgery, I had osteoporosis, multiple, multiple abscesses and fistulas. I’ve become resistant to antibiotics due to utilizing them. I’ve suffered infertility, anaemia and an awful lot of psychological distress. And quite frequently it didn’t feel like I did have my
clinicians in my corner. This is how it felt an awful lot of the time. Like I was just another patient. I felt like this was all life-changing. I felt misinformed. I felt unattractive as a woman. I was frightened. I felt stupid. I’m not going to go through all of these, but it gives you an indication of some of the negative emotions and feelings I had.
And I want to talk to you a little bit about spoon theory. So this is a way of explaining some of these difficulties. It’s a theory that was created by Christina, and M Andino. She tried to come up with a way to explain to a friend over dinner how lupus made her feel. She tried using spoons from tables around them as props, using them to explain the little things. That can be a huge hurdle for those who struggle with chronic illness or any illness. So I’m going to talk you through how my day might be using spoons. So I get up and I get my son up and have breakfast and I lose a spoon. I take my son to nursery. I come home, I make a cup of tea, and I sit at my desk. Another spoon is gone. I sit through two meetings, contributing ideas and thoughts. Another spoon is gone. I make lunch and I drink something healthy and digestible. I lose a spoon. I work on a document, maybe for an hour or two, paying attention to detail and adding some content. That’s another spoon gone. I present at a meeting and answer questions on the project. I need to lose a spoon. I then take the dog for a walk with another spoon. Now I’m getting towards the end of my day and I’ve only got one spoon left. So I would have loved to have dinner with my husband tonight or go out with my work team for drinks. But I’ve got some decisions to make and I still have someone to pick up from nursery. So that’s my decision made.
And when I run out of spoons, I’m often really exhausted or I’m in pain and I can’t buy more spoons or pluck them from thin air. I can take one from the next day, but then I start with fewer spoons tomorrow. Now healthy people get dozens of spoons and I might only get five or I might get nine. And people with other conditions might only get this metaphor not to give a lecture on the finer points of cutlery, but to let you know that having a chronic illness that others can’t see is about making difficult decisions every day about what you can get done without wanting to offend anyone or seem less of a team player. And people like me constantly consider how to use our spoons so that we can be the very best we can be. So if we can’t go for a drink after work or stay for a long time at the eight at the office, or stay all day at the staff conference because of the number of spoons will use, standing all the way home on a peak-time train is huge. I would say stick with us. Be understanding because people with illnesses like me are making difficult choices to fail and stay. Okay. But I would also say that we’re not like that all the time. So sometimes we’ve got more spoons than others. Now. Sometimes when all those spoons are gone, it can feel like this. And I have felt like this as a person many, many times.
I was told my illness would be a mild inconvenience. It has not been. But what I’ve done to combat this is learning the system and learn how to get the most out of it. However, the sad truth is that not everyone can do that, or they might have too few spoons to be able to do it. How many patients have you treated who’ve just given up because they couldn’t navigate their way through the fear, the unknowns and the pain? And now I’m hugely lucky because I had the most amazing team around me who have managed to get me through so many surgeries.
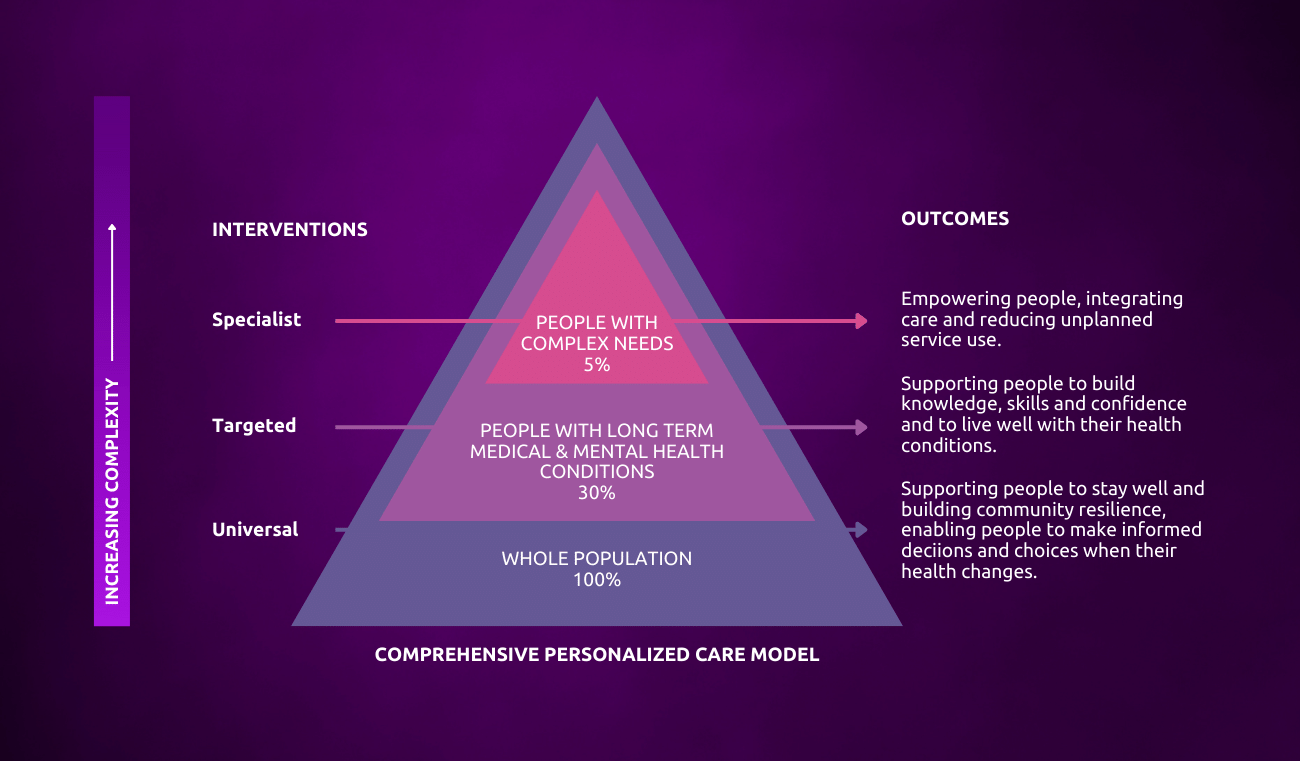
It’s an NHS England model on personalized care and it helps to establish a whole population approach to supporting people of all ages and their carers to manage physical, and mental health and well-being and build community resilience and make informed decisions and choices when their health changes. You can see the inputs on the left about specialist care, targeted care and universal care.
The types of the population you might be looking after with increasing complexity, but also the recognition that people move between groups as health changes now and then.
Finally, on the right-hand side, you’ve got outcomes, which are all about empowering people and supporting them to live well and stay well.
But I recognize having worked in the health and social care as a professional for many years, that there are also several barriers and enablers. You’ve got issues with cost and time. You know, you can’t spend hours with every patient. There are challenges with how our national payment systems are set up and how care is funded. There are organizational processes and structures, for instance, I.T. that get in the way. Sometimes leaders don’t promote patient-centred care and sometimes the culture doesn’t promote it, and actually, sometimes the patient doesn’t promote it.
I would say that you don’t know you’re doing it well a lot of the time as a professional, because every patient is different. And guess what? They’re different on different days as well. So this is not an easy thing to handle as a health care professional.
TOP TIPS FOR BETTER PATIENT EXPERIENCE
- Communication: Start with communication. I’d say just ask your patients if you’re not sure, be humble. It’s a skill that needs to be learned like any other. There’s something really important about humility and not just being a doctor and treating diseases and conditions.
- Trust: It’s really difficult for a patient to trust healthcare professionals, particularly a patient with a long-term condition like me, who’s used to building up strong, trusting relationships.
- Individualized empathy: You may get tired of hearing each person’s particular concerns or life challenges, and you might have life challenges of your own at any one time that you’re dealing with. But for that patient, that consultation is probably the biggest thing happening to them that day. They’ll watch everything you do, and hear everything you say. They’ll listen for the pauses and the tone, and they’ll interpret what it means to try and appreciate that and tailor your approach to them
Don’t preempt what you think that they might say and respond to that instead and recognize I think that it’s really hard because one size doesn’t fit all when it comes to person-centred care.
It’s really difficult to get it right for everyone. And I think also patients have to play that role, too. They need to listen. They need to engage with you and communicate and respect you as a professional. As healthcare professionals, you should be brave in asking patients, families or rescuers to play a part where it is possible.
Author
-

Head, Clinical Outcomes & PPE COVID-19 Task Force, Cabinet Office, Westminster, London



