Continuous Quality Improvement Through Clinical Indicators
Read the Magazine in PDF
Abstract
The article addresses challenges in national health services, including overcrowding and pandemic pressure. It emphasizes the importance of data display, using statistical process control charts and funnel plots. Ireland’s national quality profile initiative is discussed, focusing on patient-reported outcome measures, integrated care, and quality measures for nursing and midwifery care. Staff engagement is highlighted as vital for delivering quality care in healthcare settings.
Introduction
The health service is well-funded, but still under a great deal of pressure. Overcrowding in the emergency departments is a common issue, and it’s not a dignified situation for patients. Healthcare workers are working tirelessly to overcome this problem, especially during the pandemic. The case numbers over the last year reflect the struggles faced during this time.
Challenges in Health Service
Healthcare workers face exhaustion due to pandemic demands. Quality improvement programs are implemented, but care compartmentalization is challenging when patients may have undetected COVID. Intensive care units still experience pressure despite a stable third wave. Ireland has a successful vaccination program and promotes global vaccine equity. Overemphasis on measurement can hinder quality improvement efforts, though it remains crucial for evaluating effectiveness. Deming’s quality improvement methods are vital for structured improvement processes.
In Ireland, addressing health disparities among sub-populations like the traveling community is crucial, requiring improved data and intelligent visualization methods. Utilizing statistical process control charts and funnel plots can help communicate care effectiveness and identify areas for improvement. Presenting data in tables with indicators lacks trend analysis over time, leading to potential overreaction and unnecessary changes without statistical controls.
The Need for Measurement
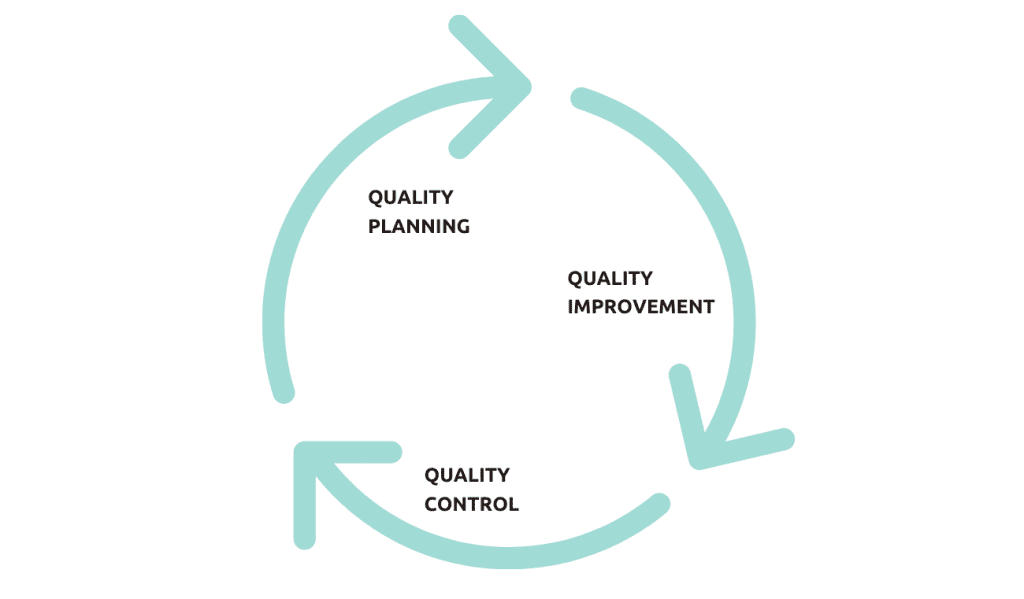
The Juran Trilogy highlights when to measure quality: during planning, improvement, and continuous monitoring for sustained improvement. Measuring integrated care involves assessing structure, process, outcomes, and culture.
It’s challenging but crucial to measure the care environment’s culture. Prioritize actionable measures in public health, share data transparently, and focus on trends over assigning blame. Analyzing and visualizing data effectively is vital for successful healthcare improvement.
There are some common pitfalls when it comes to measurement:
- Trying to improve something that doesn’t require improvement or is beyond our control.
- Neglecting expertise can lead to flawed improvement projects.
- Setting arbitrary targets can lead to game-playing and tunnel vision (neglecting other measures that lack targets).
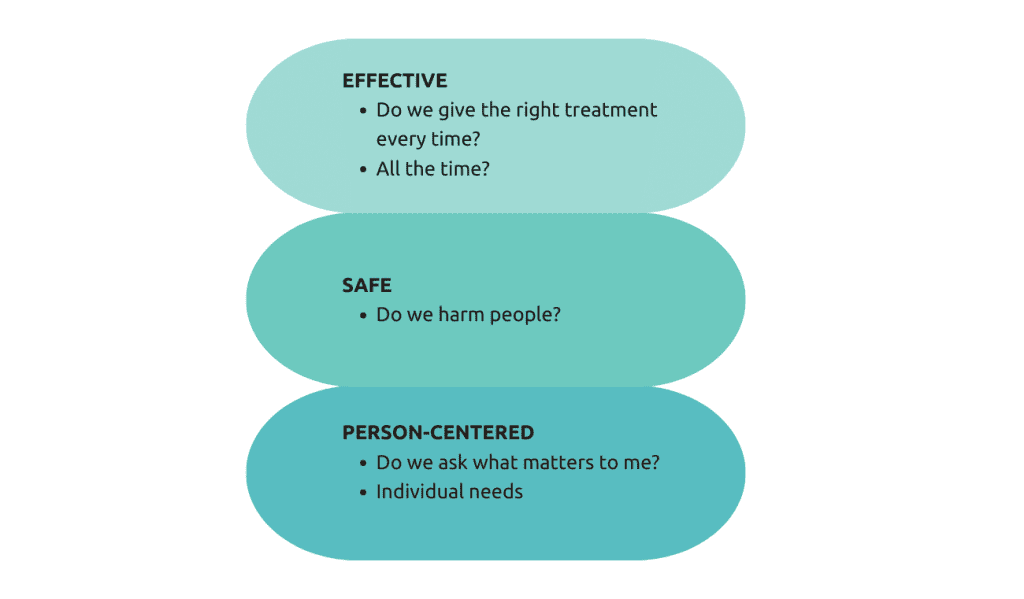
To measure patient care quality, use valid, reliable, and consistent measures across institutions, aligning with safety, efficiency, care, and patient focussed. Consider feasibility and burden on healthcare services. Involve patients in defining relevant measures that matter to them.
Using clinical quality indicators in practice
Performance report data can be misleadingly displayed, questioning the need for certain measures.
- We had physiotherapy access targets that we could not meet and then they were adjusted downwards to match actual performance, without any access improvement.
- Clinical indicators can be misused, prioritizing certain measures over things that directly impact patient care.
Different levels of measurement for improvement
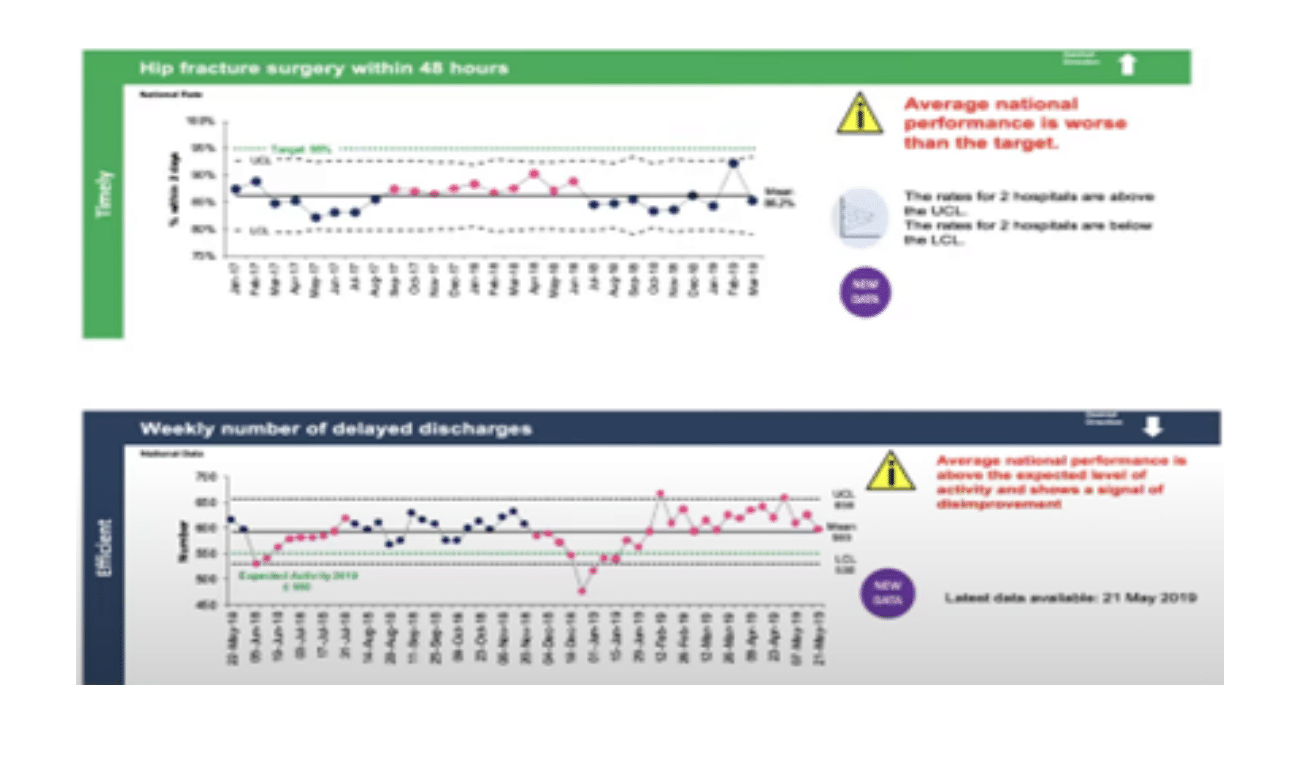
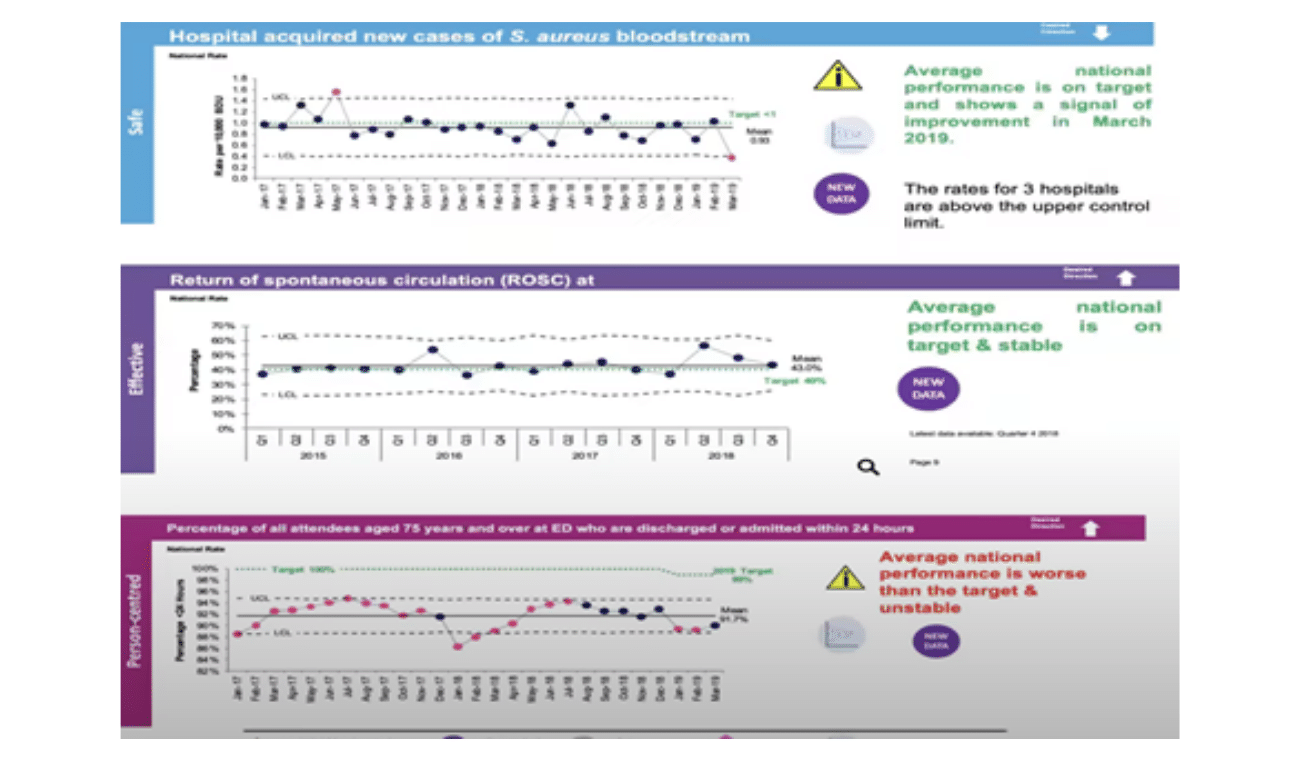
In Ireland, quality improvement efforts involve using PDSA cycles to test changes on a small scale and then implement them more broadly. The national quality profile initiative uses statistical process control charts and funnel plots to identify special cause changes and variations, promoting informed decisions and interventions to improve care. The data is displayed intuitively, allowing healthcare leaders to track progress and take action accordingly. Examples from the quality profile show trends in staff bloodstream infections and cardiac arrest outcomes, driving improvements in patient care. Measures like hip fracture surgery timing and delayed discharges are also monitored to address issues and ensure quality care.
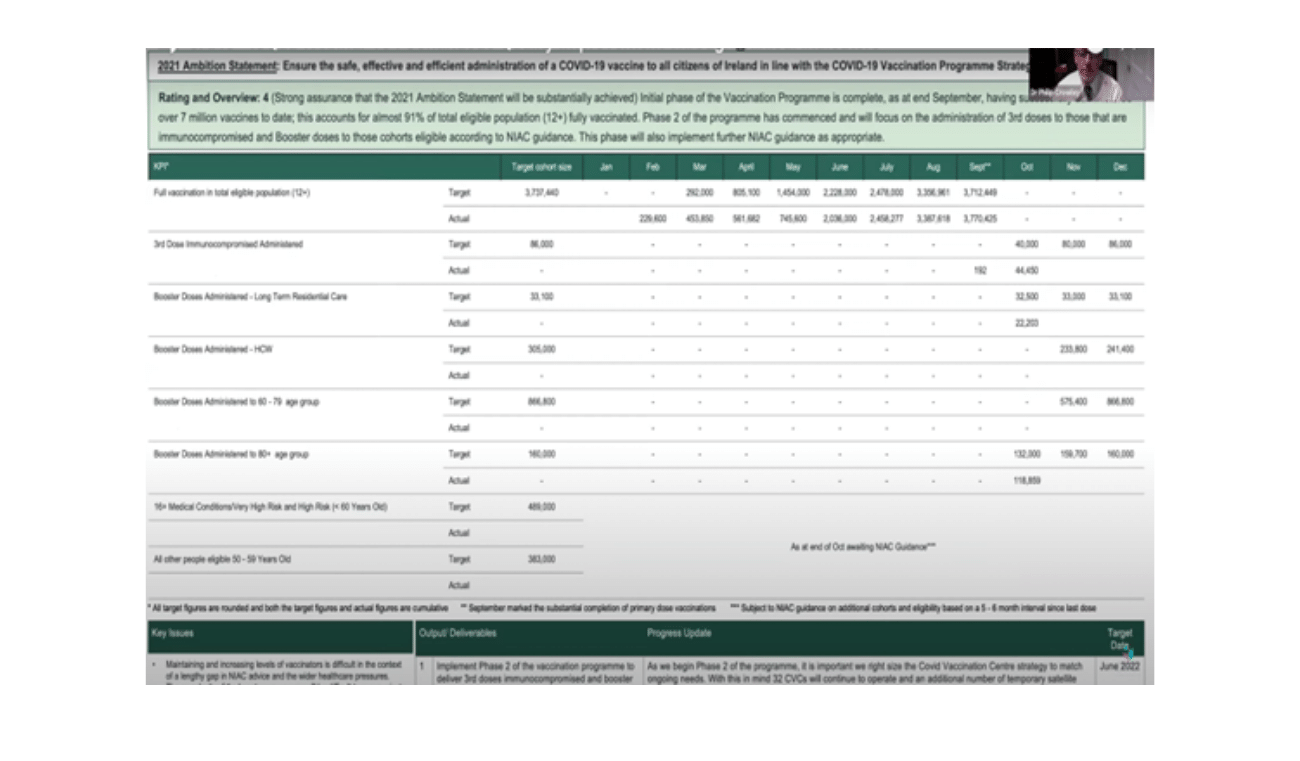
The quality profile in Ireland is shared with the National Health Service board, the Department of Health, and the public. Strategic scorecards highlight areas of action and investment commitments with specific goals and targets. The Covid vaccination program was been successful in meeting its targets. Performance management is ongoing, with patient-reported outcome measures aiding in tailoring care to patients’ needs. Integrated care programs for older people are being implemented with measures across five domains to address the knowledge gap in care quality. Performance measures are reported to identify poor performance and collaborate for improvement.
Proms include:
- Mobility
- Self-care ability
- Pain
- Discomfort
- Emotional well-being
Strategic Scorecard
In Ireland, multiple data sources are drawn together in a single document the Strategic scorecard. This gives a snapshot but comprehensive view of progress against agreed annual priorities and is used to call services to account for performance.
The health service in Ireland is incorporating a new outcome measure based on patient experience. Nursing colleagues have access to various quality measures, including quotes from nurses and midwives, to assess and improve care quality.
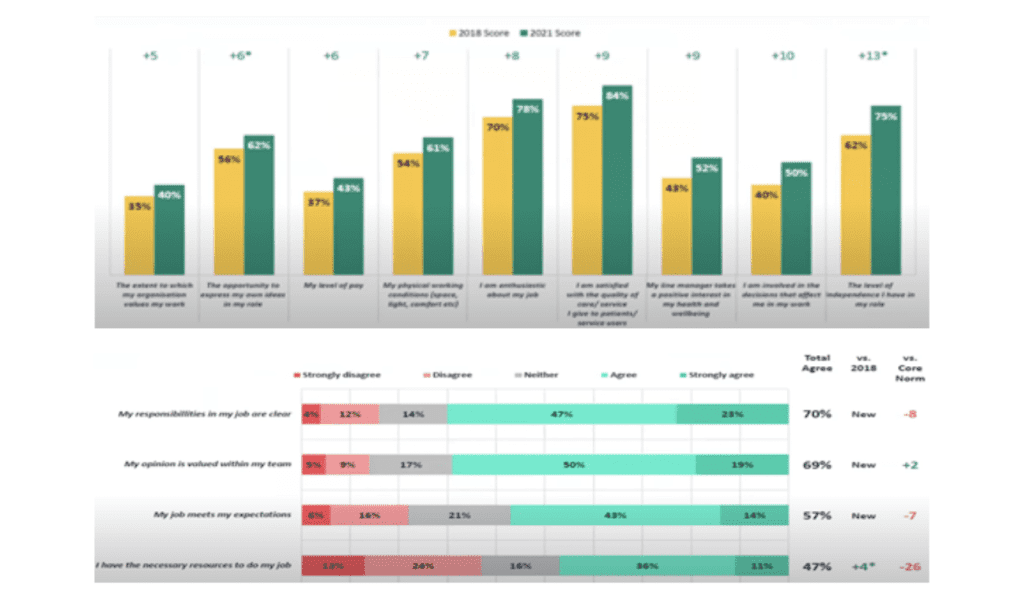
Staff survey
Staff engagement is essential, and there are efforts to gather frontline staff opinions through surveys and forums. The recent staff survey revealed an increase in the number of staff feeling valued, but improvement is still needed. The survey helps gauge workplace culture and identify areas for improvement, with tailored results for specific organizations. Other measured metrics include job responsibilities’ clarity. The goal is to create a safer environment for patients and improve overall service quality.
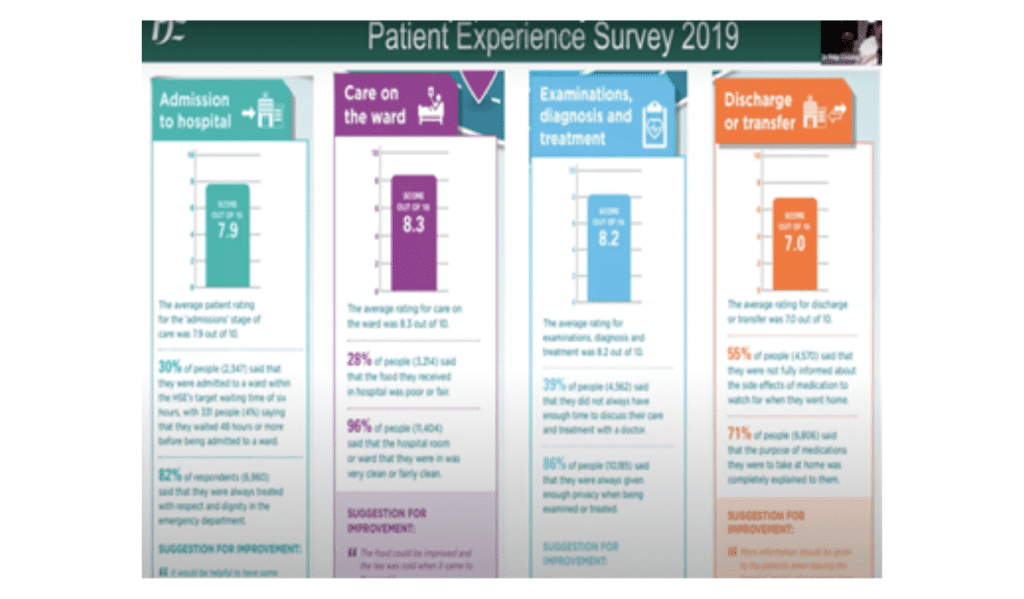
Patient experience survey
There are also patient experience surveys conducted annually to measure various aspects of their hospital admission such as clarity on admission purpose, respectful treatment, and quality of care.
For example, in 2019, 28% of patients reported poor or fair quality of food. While 72% rated it as good, it is essential to address the concerns of the remaining 28%. Similarly, 96% rated the hospital’s cleanliness as very or fairly clean, which is positive. The surveys also include quotes from patients to provide more context. These measures are specific to each healthcare institution, enabling them to identify areas for improvement and compare themselves to national averages.
The survey captures patients’ qualitative feedback, including quotes about their experiences and preferences. Data and stories both play vital roles in understanding situations. During the pandemic, staff experiences were monitored, showing mixed feelings. Managers enable staff to make decisions, leading to positive outcomes. The “epidemiology of kindness” promotes employee flourishing and inclusivity, crucial for staff morale. A highly effective healthcare service values and supports all employees, ensuring patient preference.
In this experience my treatment was most influenced
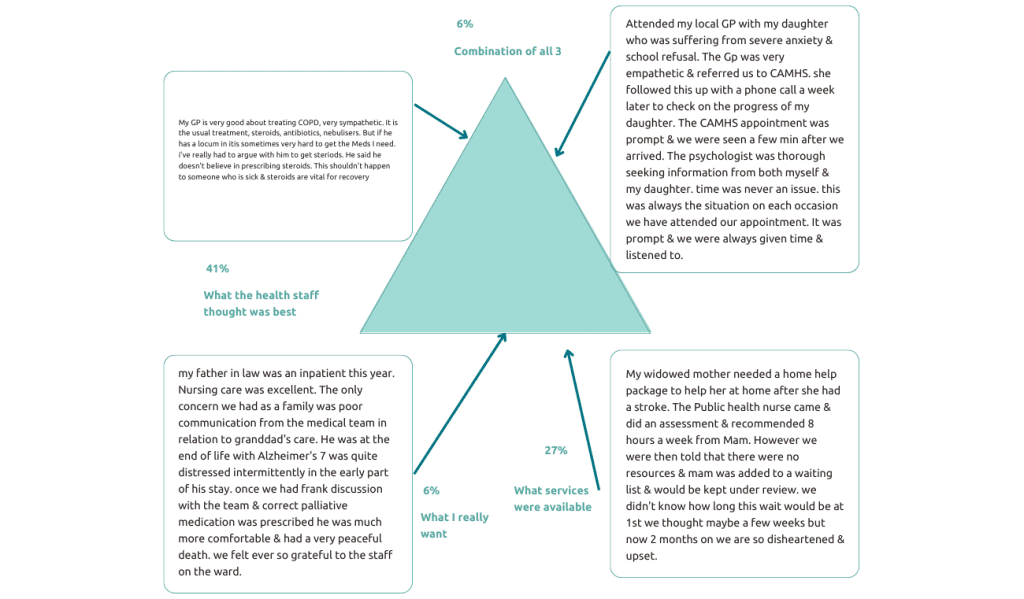
Michael West, a professor at King’s Fund London, advocates for distributed leadership that empowers frontline staff to deliver their improvements.
Conclusion
The Irish national health service faces significant challenges, and quality improvement and measurement are vital tools for addressing them. The Institute of Medicine’s domains of quality offers a comprehensive framework for evaluating care, while effective data visualization enhances understanding and decision-making. Patient-reported outcome measures and integrated care programs promote personalized and patient-centered care. The assessment of nursing and midwifery care, coupled with staff engagement, ensures a safer environment for patients. The annual staff survey helps gauge workplace culture and identifies areas for improvement.
By making the quality profile public, transparency is promoted, encouraging collaboration and progress. Together, these efforts contribute to enhancing patient care and achieving better health outcomes for all. To create a culture of improvement, it is important to only measure what matters, involve patients and clinicians in deciding what to measure, and use evidence-based patient-related outcomes. It is also essential to build capability for measurement, use existing data, seek transparency, and avoid blaming staff. The goal is to create a culture that values and supports staff while fixing problems that arise.
FAQ
Q: What is one of the issues that arise when trying to benchmark?
A: When trying to benchmark, one issue is truly comparing apples to apples. Ratios can be derived differently between organizations and have different denominators and nominators.
Q: How can benchmark measures be made truly comparable between organizations?
A: Standardization is key to making benchmark measures comparable. This can be achieved by training people together to agree on how data is collected and measured equivalently.
Q: How does one decide the denominator for a measurement?
A: The denominator for measurement depends on the level being measured. For population measures, you decide what part of the population you’re measuring and then work out how many people are in that denominator. In a hospital, you decide which types of patients to include and exclude, and then agree with all other units to include the same patients.
Q: What is the appropriate period to analyze data using SPC charts?
A: SPC charts should be analyzed after at least six months of data has been collected. It is generally recommended to measure things month by month rather than week by week, and it is better to wait until closer to nine months to start acting on the data.
Q: How should benchmarking be done? Who should make the target and based on what?
A: When benchmarking, it is important to set a stretch target that is reasonable and agreed upon by the clinical community and patients. The target should not be so high that it demotivates people, but it should not be so low that it is already being met.
Author
-

National Director of Strategy and Research, Health Services Executive, Ireland



