Quality Tools
Read the Magazine in PDF
Abstract
The article highlights the importance of a comprehensive toolbox for healthcare professionals to improve patient care. It emphasizes the involvement of patients and their families in creating quality healthcare. Professionals are encouraged to use frameworks to address issues effectively and continuously improve care. The model for improvement helps set clear criteria and measure interventions’ effectiveness. Embedding improvements and preventing regression require prioritizing improvement, generating evidence, and collaborating with patients and families to consider their needs and resources. The ultimate goal is to enhance the quality of healthcare for patients and their families.
Introduction
The article explores a fresh perspective on using tools to improve healthcare quality, focusing on understanding the context for their effectiveness. It aims to boost confidence in taking action to enhance healthcare quality for patients and teams. Emphasizing co-production with patients, the article highlights the importance of shared ownership and responsibility for healthcare issues. The ultimate measure of success should be the outcome for patients and their families, aligned with their wishes and support needs.
Tools
The analogy of a toolbox reminds us to be flexible and use various tools for different situations in healthcare. Quality care requires conscious and conscientious choices, considering the unique needs of each patient. Striving for quality involves action-based efforts, engaging both our minds and hearts to benefit our colleagues and patients.

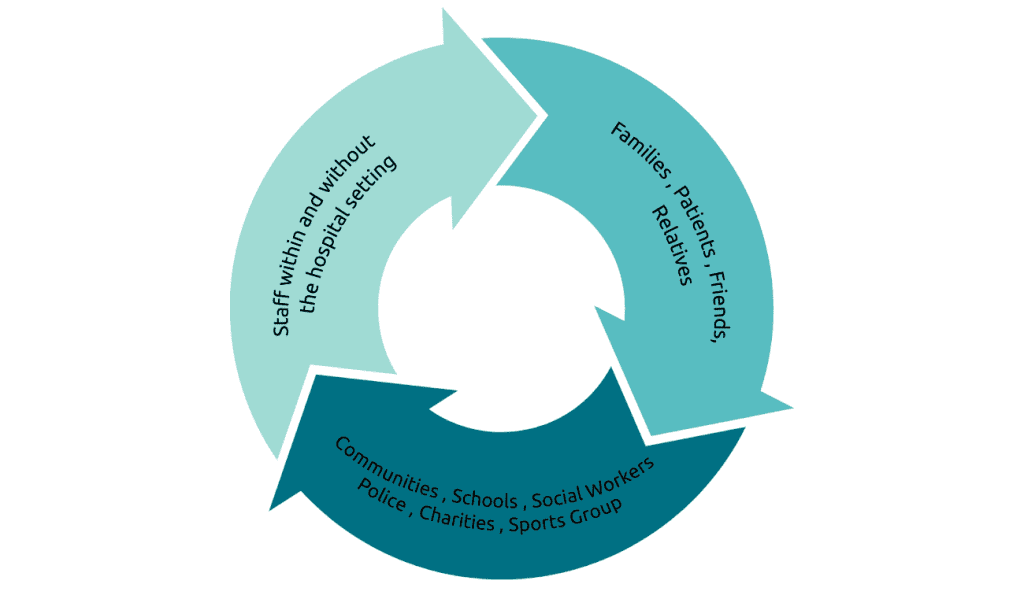
Involving the entire healthcare system, including various stakeholders, is crucial for creating quality healthcare. This includes clinical staff, communities, schools, social workers, local authorities, and patients and their families. Failing to involve the entire system may lead to diminished quality of care, so it’s vital to engage as many stakeholders as possible.
Complexity
The complexity of healthcare work requires us to understand the impact of various factors such as technologies, patient conditions, team dynamics, and the work environment. We must work within this complexity to engineer optimal patient outcomes and provide effective care. Simple solutions or toolkits may not suffice, and we must recognize and embrace this reality to ensure optimal care delivery and value to patients and organizations.[1]
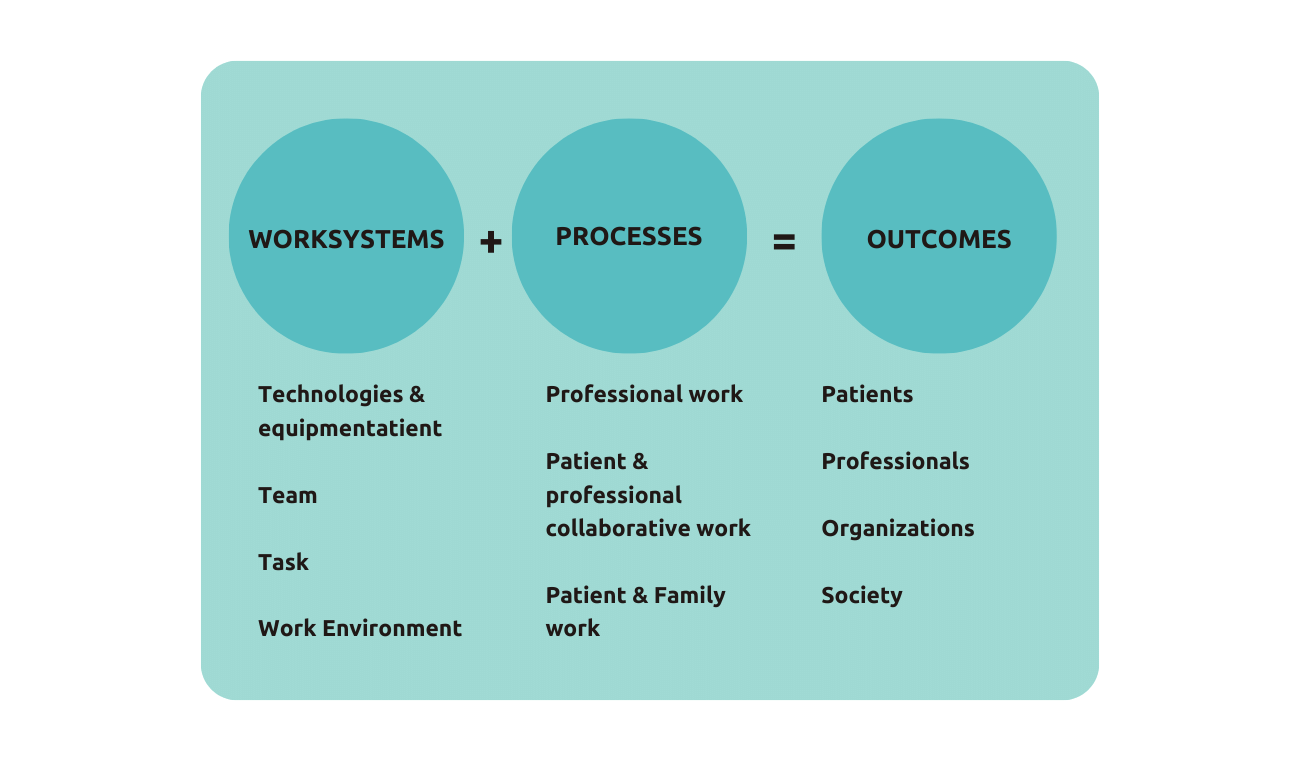
In the study, “SEIPS 3.0: Improving Patient Safety Through Human-Centered Design”. Carayon et al. propose SEIPS 3.0, an updated model that integrates Human Factors and Ergonomics (HFE) into healthcare quality and patient safety improvement.
The new model expands the process component by using the patient journey concept to capture patients’ interactions with various care settings over time and space. SEIPS 3.0 aims to enhance patient safety by providing a comprehensive understanding of complex healthcare systems.
It presents challenges in considering multiple viewpoints and ensuring genuine participation at the interface, offering valuable insights for HFE researchers and professionals.

How do we start?
To improve care quality, start by examining the current system and the quality of care provided. One should read Charles Vincent and Rene Amalberti’s framework, which helps to identify the areas for improvement. Use the optimal care versus sub-optimal care grid to assess if care is consistent with standards and whether there are gaps or unreliability. Address imperfections to optimize current processes.
If harm occurred, a systems-wide approach is needed to rethink the entire system and enhance collaboration among healthcare professionals and patients. Consider the work system, professional system, and patient collaboration to deliver reliable care.[2]
Improvement Methodology
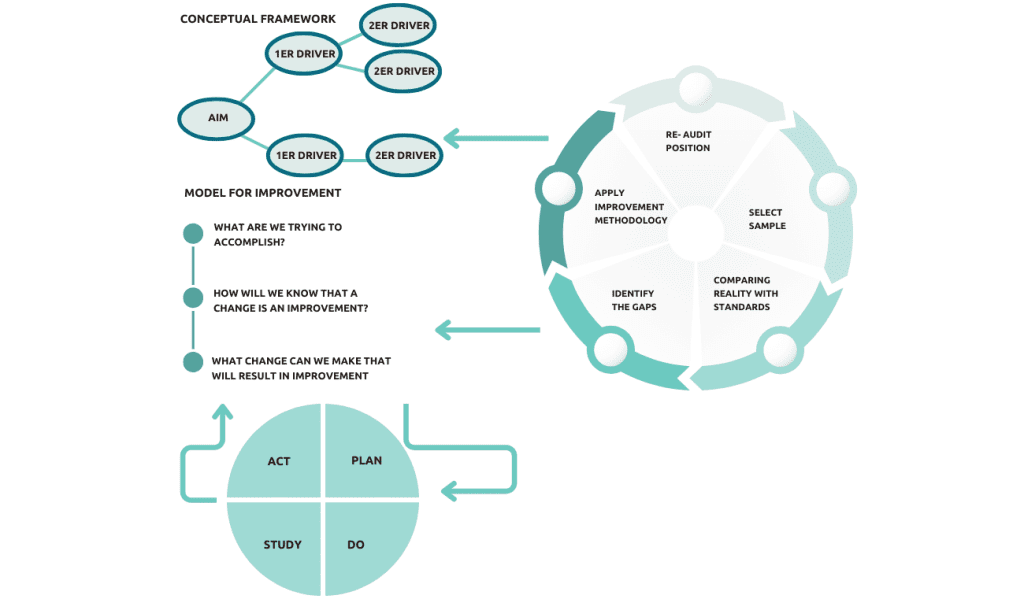
To improve care, start with establishing a standard and comparing it to day-to-day work to identify gaps.
Use improvement methodologies intelligently, involving relevant stakeholders and considering system variation. Measure the impact of implemented ideas to ensure positive outcomes and embed changes for long-term success. Collaboration and sharing evidence with skeptics is crucial for ongoing improvement.
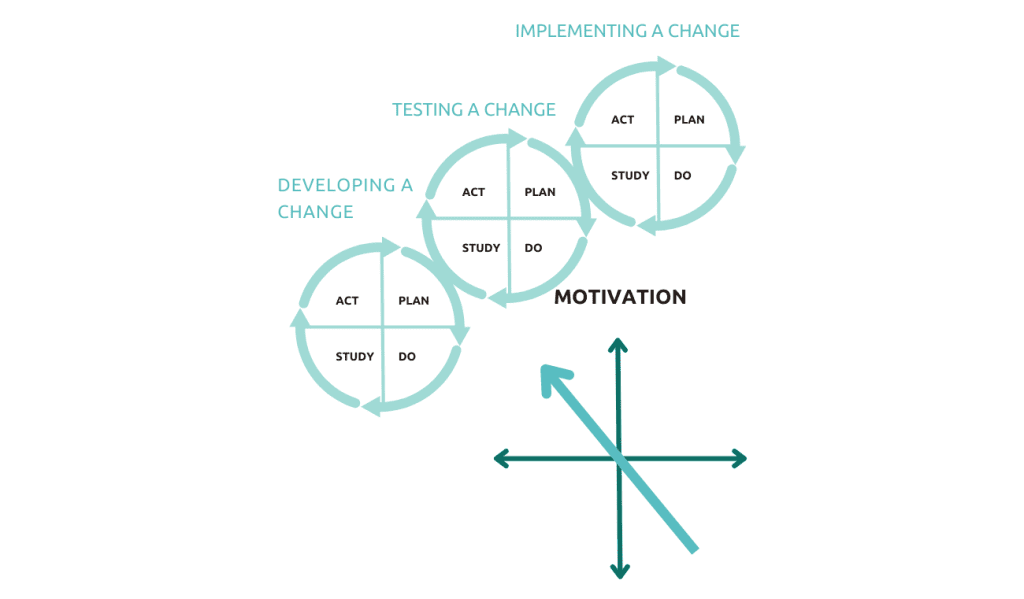
Improvement methodologies encompass various considerations and require a holistic approach. The Front-Line Plan-Do-Study-Act (PDSA) cycle is a key foundation for these methodologies, emphasizing testing ideas in real-world settings for sustainable improvements. Having tools alone isn’t sufficient; understanding the system, involving the right people, and generating team energy is essential for successful and lasting improvements in patient care.
How can we approach the first three steps of the sequence – understanding the system, identifying variation, and involving stakeholders?
To initiate improvement, gather informal input, and conduct a fishbone analysis to identify areas for enhancement. Understand system variation through small audits.
Involve stakeholders, fostering ownership and conceptualizing actionable steps for a collaborative effort. Determine actions and engage relevant team members to achieve a sustainable shift in performance.
Model for improvement
To improve patient outcomes, start with the model of improvement, clarifying goals for professionals and patients. Measure impact with specific indicators like fever reduction or improved cardiac function. Test manageable ideas in small trials, then adopt, adapt, or abandon based on results.
Use tools like Lean or 5S for documentation and process mapping to identify improvement areas. Involve patients directly or indirectly through the microsystems approach, seeking their feedback and observations to optimize their experience. The ultimate purpose is to enhance patient outcomes and ensure meaningful improvements in healthcare.
Measuring Improvement
Implement a concise Plan-Do-Study-Act (PDSA) cycle that can be easily tested with a small group of patients. Predict expected changes to ensure a grounded and ethical plan. Modify the cycle as needed, keeping records and taking measurements regularly for improved system performance. Prompt and explicit progress tracking maintains motivation and helps stay invested in the changes being made.
To ensure successful improvement, consider unintended consequences and measure progress across the system. Frequent measurement provides evidence and keeps motivation high.
Regular assessment ensures learning and continuous improvement in healthcare practices, benefiting patients and professionals alike.

Embedding Improvement
To embed improvements, prioritize improvement in the structure and environment, fostering positivity and personalization. Generate evidence through patient feedback and data to convince skeptics and inspire confidence.
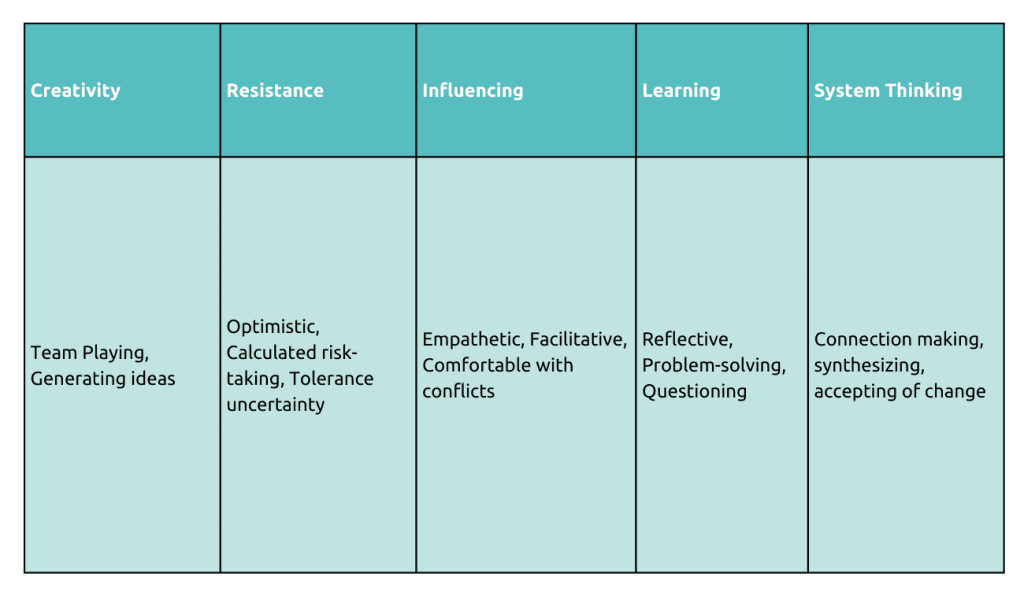
Professionals play a crucial role with attributes like curiosity, empathy, and optimism, ensuring the best care for patients. Enhancing personal attributes supports each other and improves patient care in the short and long term.
Collaborate with teams and organizations to spread knowledge and enthusiasm. Publish results to share successes with others. Engage patients and families at every step, considering their needs and perspectives. Empower patients to be active participants in their care.
Professionals play a crucial role with attributes like curiosity, empathy, and optimism, ensuring the best care for patients. Enhancing personal attributes supports each other and improves patient care in the short and long term.
To ensure successful improvement, consider unintended consequences and measure progress across the system. Frequent measurement provides evidence and keeps motivation high. Implement a concise Plan-Do-Study-Act (PDSA) cycle that can be easily tested with a small group of patients. Predict expected changes to ensure a grounded and ethical plan. Modify the cycle as needed, keeping records and taking measurements regularly for improved system performance. Prompt and explicit progress tracking maintains motivation and helps stay invested in the changes being made. Regular assessment ensures learning and continuous improvement in healthcare practices, benefiting patients and professionals alike.
Conclusion
Providing quality healthcare requires a well-organized toolbox equipped with various tools, and we must use them consciously and conscientiously. We need to involve the entire system, not just clinical staff, in creating quality healthcare. Healthcare is complex, and we must acknowledge this reality to ensure that we can deliver optimal care and value to our patients, organizations, and society.
To begin, we should conceptualize tool usage by considering what’s happening in the current system and examining the quality of care being provided. Improvement methodology involves understanding the system, ensuring that all relevant stakeholders are involved, and measuring the impact of the ideas we put into practice. Enthusiasm, embedding changes, and sharing evidence are also key to continuous improvement.
Author
-

Board Member and person-centred Care expert, ISQua, Associate Clinical Director for Patient Safety, West of England Academic Health Science Network



