Best Practices to Prevent Needlestick Injuries
Read the Magazine in PDF
Introduction
Needles are unavoidable in healthcare settings, but needlestick injuries are preventable. A needlestick injury is a penetration of the skin by a needle or other sharp object that has been in contact with another person’s blood, tissue, or other body fluid before the injury [1] (OSHA 2001; CDC 2011). Needlestick injuries (NSIs) remain a global threat, with an estimated 44.5% of healthcare workers experiencing at least one occurrence annually.
The World Health Organisation (WHO) reports that over 2 million occupational exposures among 35 million healthcare workers (HCWs) occur each year, making NSIs one of the most dangerous occupational hazards for HCWs worldwide.[3] (WHO, 2019).
Impact of needlestick injuries
Threat of contracting infection
In fact, after a needlestick injury, almost any organism can spread, although very few of these types are clinically significant. The most significant pathogens that may be contracted following a needlestick injury are hepatitis B, hepatitis C, and HIV.
According to CDC [4], the risk of transmission for bloodborne infections after needle-stick/cut exposure to infected blood is 0.3% for HIV, 2.7–10% for HCV and 6–30% for HBV [depending on the hepatitis B e antigen (HBeAg) status]
Economic implications
NSIs involve potential risks, upfront expenses for laboratory testing, treatment costs, post-exposure prophylaxis for registered nurses, and financial burdens for hospitals due to staff absences5. Following an NSI, significant expenses include testing for infection, post-exposure prophylaxis, short- and long-term treatment of chronic viral infections, staff absence and replacement, counselling for injured workers, and legal consequences [6]. An estimated $6.1 million in France and $118-591 million in the USA are spent annually on NSI diagnostics and treatments as of the year 2007. In Mumbai, India, a tertiary care hospital was paying around ₹ 9000 / HCW / episode for needlestick injuries as short-term costs as of the year 2010 which could be more costly considering the year 2023. [7,8,9]
Psychological implications
Needlestick injuries in healthcare settings can cause significant psychological distress, including fear of bloodborne infections like HIV or Hepatitis B, guilt, and self-blame. These injuries can lead to increased vigilance and hypervigilance, negatively impacting job performance and overall well-being. Healthcare organizations should prioritize providing support systems for individuals experiencing needlestick injuries, including counselling services and education on prevention strategies. Recognizing these implications and providing appropriate support systems is crucial to mitigate their long-term effects on mental health [10 ,11].
Impact on patient care
Needlestick injuries in healthcare workers can cause increased anxiety, stress, and absenteeism, leading to suboptimal patient care. This can result in a lack of continuity of care, disrupting effective patient management. Additionally, needlestick injuries increase the risk of bloodborne infection transmission, posing a direct threat to patients’ health and undermining trust in the healthcare system. Therefore, it is crucial to address these issues to ensure patient safety.
Prevention of Needlestick injuries
Education and training
Training on needlestick injuries is crucial for healthcare professionals to prevent incidents and ensure safety. It educates workers about the risks of needlestick injuries, such as bloodborne pathogens, and equips them with practical skills to prevent them. Training also fosters a culture of safety within healthcare organizations, encouraging open communication and prompt reporting of incidents. Regular training leads to more consistent adherence to safe practices.
Administrative and Engineering controls
Use of safety-engineered devices that incorporate features like retractable needles or protective shields can significantly reduce the risk of accidental needlesticks. Employers must provide these devices and ensure their availability in all areas where sharps are used.
Types of sharps safety devices that can be used to protect workers:
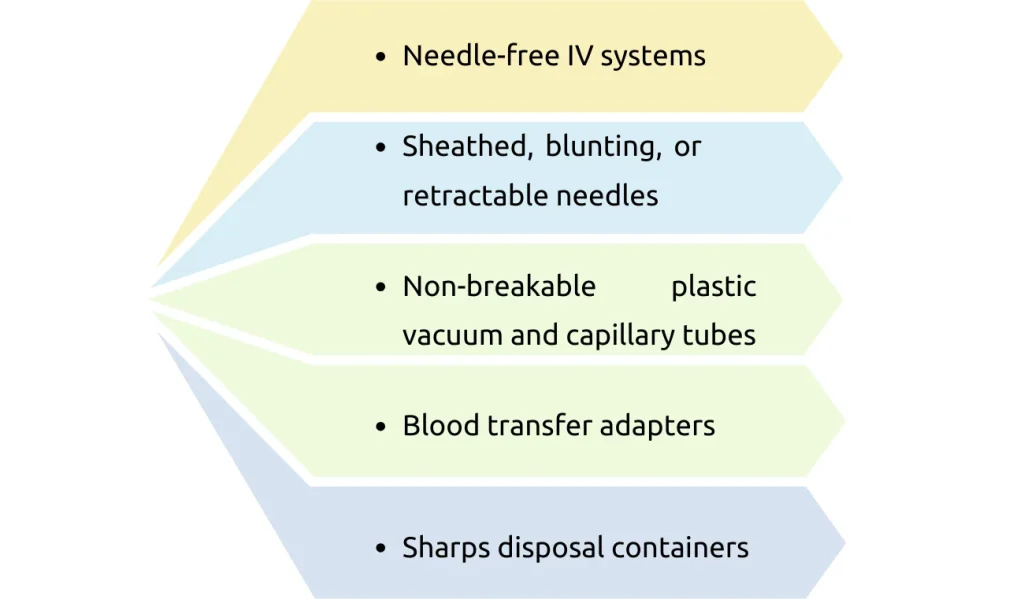
Studies show that needlestick injuries may have increased after the implementation of Special Safety Engineered Devices (SEDs), with the most common causes being difficulties in operating the device and improper needle disposal, contrary to the expected decrease in needlestick injuries [12]. So it is important that employers involve frontline workers in selecting devices with safety features and train them adequately on the use of SEDs.
Strict infection control practices
The prevention of needlestick injuries among healthcare workers is contingent upon strict adherence to infection control protocols. The risk of these injuries can be reduced by using safe needle handling practices, practicing good hand hygiene, donning personal protection equipment (PPE), and properly segregating and disposing of waste. Consistent implementation of these measures can create a safer environment for patients and staff members.
The “One and Only” campaign emphasising “one needle, one syringe and only one time” by the CDC is an essential initiative that aims to ensure safe injection practices in healthcare settings. By emphasizing the importance of using new needles and syringes for each patient, this campaign contributes significantly to preventing bloodborne infections. It serves as a reminder for healthcare providers to prioritize patient safety while administering injections.
Guidelines from Ministry of Health and Family Welfare, India to health care providers
When the use of sharp objects cannot be avoided, ensure that the following precautions are observed[13]:
- Never replace the cap on a used needle.
- Never direct the point of a used needle towards any part of the body.
- Do not remove used needles from disposable syringes by hand, and do not bend, break or otherwise manipulate used needles by hand.
- Never reuse syringes or needles.
- Dispose of syringes, needles, scalpel blades and other sharp objects in appropriate, puncture-resistant containers.
- Ensure that containers for sharps objects are placed as close as possible to the immediate area where the objects are being used (‘point of use’) to limit the distance between use and disposal and ensure the containers remain upright at all times.
Ensure that the containers are securely sealed with a lid and replaced when ¾ full. Ensure the containers are placed in an area that is not easily accessible by visitors, particularly children. Closed, resistant shoes/footwear should be used by all individuals in the patient care area to avoid accidents with misplaced, contaminated sharp objects.
Recommendations of CDC for Healthcare Professionals
The following measures are recommended by CDC to prevent Needlestick injuries and to ensure sharp safety among healthcare professionals [14].
Be prepared
- Organize your work area with appropriate sharps disposal containers within reach
- Work in well-lit areas
- Receive training on how to use sharps safety devices
- Before handling sharps, assess any hazards–get help if needed
Be aware
- Keep the exposed sharp in view
- Be aware of people around you
- Stop if you feel rushed or distracted
- •Focus on your task
- Avoid hand-passing sharps and use verbal alerts when moving sharps
- Watch for sharps in linen, beds, on the floor, or in waste containers
Dispose of sharps with care Be responsible for the device you use Activate safety features after use Dispose of devices in rigid sharps containers; do not overfill containers Keep fingers away from the opening of sharps containers.
Culture of safety
A Facility’s “culture of Safety” is important for sharps injury prevention and the facilities that value safety have fewer sharps’ injuries. Characteristics of such facilities include:
- Sharps injury prevention is a prominent organizational priority
- Management and staff have a shared commitment to prevent sharps injuries
- Staff members are encouraged to report sharps injuries promptly
- Individual safety accountability is promoted
Conclusion
The prevention of needlestick injuries necessitates a multifaceted strategy that includes engineering controls, continuous monitoring, safety-engineered equipment, education, and training. We can successfully protect our committed healthcare professionals’ well-being while delivering the best possible patient care by applying these best practices consistently across healthcare settings.
Reference
- https://www.cdc.gov/nhsn/PDFs/NaSH/NaSH-Report-6-2011.pdf
- Bouya S, Balouchi A, Rafiemanesh H, et al. Global Prevalence and Device Related Causes of Needlestick Injuries among Healthcare Workers: A Systematic Review and Meta-Analysis. Ann Glob Health. 2020 Apr 6;86(1):35.
- WHO. Needlestick injuries. 2019; https://www.who.int/occupational_health/topics/needinjuries/en/.
- National Guidelines for IPC in HCF, 2020, National centre for Diasease control, Ministry of health and Family welfare , India
- Hassanpour Dehkordi A, Khaledi Far A. Effect of exercise training on the quality of life and echocardiography parameter of systolic function in patients with chronic heart failure: a randomized trial. Asian J Sports Med. 2015;6(1):e22643.
- Hanmore E, Maclaine G, Garin F, Alonso A, Leroy N, Ruff L. Economic benefits of safety-engineered sharp devices in Belgium – a budget impact model. BMC Health Serv Res. 2013;13:489.
- United States General Accounting Office. Occupational safety: selected cost and benefit implications of needlestick prevention devices for hospitals, GAO-01-60R. Published November 17, 2000.
- Leigh JP, Gillen M, Franks P, et al. Costs of needlestick injuries and subsequent hepatitis and HIV infection. Curr Med Res Opin. 2007;23(9):2093–2105.
- Rodrigues C. Needle stick injuries & the health care worker–the time to act is now. Indian J Med Res. 2010;131:384–86.
- Hambridge K, Endacott R, Nichols A. Exploring the psychological effects of sharps injuries sustained by healthcare workers. Nurs Stand. 2022 Feb 28.
- Hambridge K. The psychological impact of sharps injuries sustained by medical students. Br J Hosp Med (Lond). 2022;83(1):1-7.
- Schuurmans J, Lutgens SP, Groen L, Schneeberger PM. Do safety engineered devices reduce needlestick injuries? J Hosp Infect. 2018 Sep;100(1):99-104.
- https://main.mohfw.gov.in/sites/default/files/28461430151407757996_0.pdf
- Centre for Disease Control and Prevention. www.cdc.gov/sharpssafety
Author
-
Professor and HOU, Medical Nursing Unit, Deputy Nursing Superintendent and Additional Joint Secretary of Hospital Infection Control Committee, College of Nursing, Christian Medical College, Vellore



