Electronic Medication Systems: Opportunities, Challenges, and Risks
Read the Magazine in PDF
Abstract
Electronic medication systems hold promise for enhancing patient safety and healthcare quality, as demonstrated by efforts at Macquarie University’s Australian Institute of Health Innovation. The article emphasizes the importance of thoughtful design, addressing technology-related errors, and using non-interruptive alerts in decision support. Insights from studies evaluating system impact and recommendations for optimization are presented. Continuous monitoring, collaboration with end-users, and careful system modifications are crucial for maximizing the benefits of electronic medication systems in healthcare settings. The article addresses the “60-30-10 challenge” in healthcare and highlights opportunities for improving medication safety through technology.
Introduction
Macquarie University’s Australian Institute of Health Innovation has four research centres on healthcare quality and safety. Led by Prof. Jeffrey Braithwaite, the Center for Healthcare Resilience and Implementation Science and Prof. Johanna Westbrook’s Center for Health Systems and Safety Research emphasize multidisciplinary approaches and technology. Prof. Enrico Colera leads the Center for Health Informatics, while Prof. Henry Cutler heads the University Center for Health Economy. The Center for Health Systems and Safety Research collaborates with healthcare providers, consumers, and policymakers, with five research streams covering healthcare engagement, health analytics, diagnostic informatics, aged care, and medication safety.
Addressing the “60-30-10 challenge,” the centre aims to improve medication safety, considering the significant cost of preventable patient harm, which amounts to about $41 billion annually.
Study 1: “The three numbers you need to know about healthcare: the 60-30-10 Challenge”. Healthcare faces a persistent 60-30-10 challenge, with 60% of care following guidelines, 30% being wasteful, and 10% causing harm. Linear change approaches have been insufficient. Instead, a dynamic learning health system using AI, genomics, and patient preferences is proposed to improve decision-making and reduce waste and harm. Encouraging innovation’s diffusion will aid its adoption.
Challenges and Opportunities in Healthcare Systems
Efforts at Macquarie University’s Centre for Health Systems and Safety Research focus on the transformative impact of information technology on medication safety. They centre on optimizing clinical decision support in electronic health systems, like electronic medical records and prescribing systems.
Australia has made strides in adopting these technologies in hospitals, but challenges persist in fully realizing their benefits. Automation and computerization offer promising interventions for healthcare quality and safety. However, implementing these interventions poses difficulties. The objective is to identify and address these challenges, ensuring the successful integration of technology into healthcare systems. Ultimately, their work aims to enhance patient safety and healthcare quality, leveraging technology’s potential through innovative research in collaboration with various stakeholders in the healthcare sector.
Study 2: “The Promise of Electronic Records Around the Corner or Down the Road?” In 2009, the US Congress passed the HITECH Act, providing financial incentives to healthcare providers adopting and using electronic health records (EHRs). The act aims to improve the US healthcare system, which currently falls short of expected safety, quality, and efficiency standards. Policymakers believe EHRs will be instrumental in transforming healthcare for the better.
Electronic Medication Management
Study 3: “Short-and long-term effects of an electronic medication management system on pediatric prescribing errors” This study assesses the effectiveness of an electronic medication management (eMM) system in reducing prescribing errors in pediatrics. Short-term results show no change in overall error rates but a 62% increase in potential adverse drug events (pADEs). One year after implementation, errors declined by 36%, which included a reduction in pADEs, with a focus needed on reducing dose errors. Common error types that accounted for 90% of mistakes had wrong dose errors, after eMM, despite the system’s pediatric dose calculation features. Results may vary by setting, as demonstrated in previous research in adult hospitals showing significant reductions in prescribing errors.
Challenges with Electronic Medication Systems
The electronic medication system improves order documentation, particularly in handling unclear orders and meeting legal requirements. Study data from Australian hospitals shows impact on clinical errors is less in adult settings than in pediatrics, highlighting the need for tailored systems.
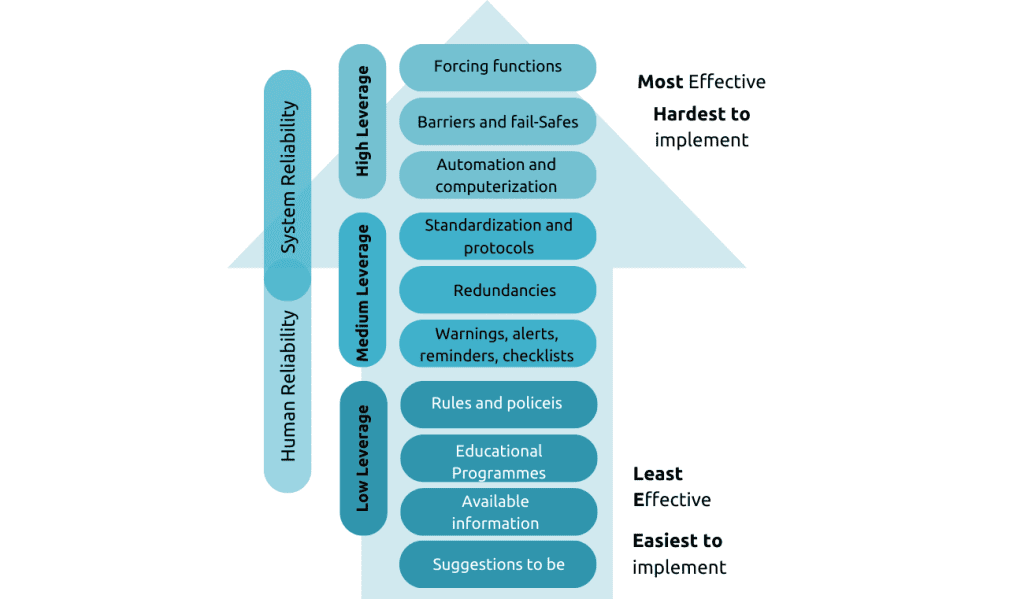
Technology-related errors persist post-implementation and account for a significant proportion of medication errors (6% to 78%). Understanding the underlying mechanisms of technology-related mistakes is crucial for patient safety. One common mechanism is selection errors in drop-down menus. Reorganizing and prioritizing items in drop-down menus can effectively address this issue.
Several selection errors were identified in the electronic medication system, leading to inappropriate doses and dosing errors. Errors included choosing the wrong route of administration for an antibiotic, dosing errors with ibuprofen due to poor prioritization in the drop-down menu, and issues with cephalosporin antibiotics. Recommendations to address these errors include displaying medication names only after entering at least five characters and prioritizing commonly prescribed options in the drop-down lists. In the adult context, a study highlighted selection errors as the most frequent technology-related error mechanism, with differences in error rates between the Med Chart and Cerner systems due to design variations.
Study 4: “Effects of Two Commercial Electronic Prescribing Systems on Prescribing Error Rates in Hospital In-Patients: A Before and After Study” This study evaluated the effectiveness of two commercial electronic prescribing systems in reducing prescribing error rates and introducing new types of errors. The e-prescribing systems significantly reduced error rates in the intervention wards, including serious errors, which decreased by 44%. However, clinical error rates showed limited change. System-related errors were observed and need further attention for system redesign and user training.
Understanding Technology related errors
Understanding the mechanisms of technology-related errors is vital to preventing their occurrence in electronic medication systems. Recent research comprehensively classified seven main categories with multiple subcategories for these error mechanisms. Feedback to pediatric hospitals on technology-related errors led to system modifications, enhancing safety. Automation improves safety through prepopulated fields in medication orders, but addressing potential drawbacks and automation bias is necessary. The study showed varying proportions of technology-related errors due to evolving electronic systems. Common mistakes include selection errors, such as choosing the wrong option from drop-down menus. System modifications like removing contraindicated routes and displaying medication names after entering characters help prevent such mistakes. The study revealed that Cerner’s order sentence feature reduced errors compared to Med Chart’s long-hand prescribing.
Continuous improvement is crucial to optimizing patient safety and preventing technology-related errors in electronic medication systems.
Study 5: “Some Unintended Consequences of Information Technology in Health Care: The Nature of Patient Care Information System-related Errors” Medical error reduction is a global concern, and patient care information systems (PCISs) are seen as a potential solution. Researchers from the US, The Netherlands, and Australia conducted separate studies on PCIS implementation. Surprisingly, PCISs sometimes contribute to errors instead of reducing them. The authors identify two main error categories: those related to information entry and retrieval and those affecting communication and coordination. With increased awareness, informatics professionals can design and implement PCISs to avoid unintended consequences and mitigate these subtle, silent errors.
Study 6: “Prevalence of computerized physician order entry systems–related medication prescription errors: A systematic review” This systematic review examines medication-prescription errors related to computerized physician order entry (CPOE) systems, assessing their prevalence and underlying mechanisms. Fourteen studies were included, with a median majority of CPOE-related errors of 26.1%. “Wrong dose” (median 31.5%) and “wrong drug” (median 26.1%) were the most frequently reported errors. Continuous reporting of these errors is crucial to improving medication safety.
Study 7: “Medication errors related to computerized provider order entry systems in hospitals and how they change over time: A narrative review” Evaluations of computerized provider order entry (CPOE) systems have shown reductions in certain medication errors along with the emergence of system-related errors. This review examines the literature on system-related errors in relation to the length of CPOE use. Thirty-one studies were analyzed, revealing that system-related errors persist over time, likely at a reduced rate. However, no study specifically explored how these errors change over time. Understanding the dynamics of system-related errors is crucial for effective prevention and mitigation strategies.
Study 8: “The safety of electronic prescribing: manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals” This study aimed to compare system-related errors in two electronic prescribing systems (e-PS) and assess their rates and manifestations. The audit of 629 inpatient admissions in Sydney hospitals using CSC MedChart and Cerner Millennium e-PS revealed that 42.4% of prescribing errors were system-related. While MedChart had more selection errors, it had fewer new task failures compared to Cerner e-PS. These system-related errors were frequently undetected, and e-PS designs with fewer drop-down menu selections were suggested to reduce error risk. The study highlights the need for better error detection and the consideration of design features to minimize the risks associated with electronic prescribing systems.
Study 9: Automation bias in electronic prescribing This study found evidence of automation bias (AB) in e-prescribing, leading to omissions and commission errors. Correct CDS reduced omission errors, while incorrect CDS increased them. Task complexity and interruptions had no impact on AB. Verification of CDS alerts is crucial to avoiding errors and ensuring patient safety. Clinicians should remain vigilant and verify CDS recommendations to mitigate potential risks.
Design Considerations and Nudges for Decision Support
Study 10: Computerized clinical decision support systems and absolute improvements in care: meta-analysis of controlled clinical trials Clinical decision support systems (CDSS) show small to moderate improvements in targeted care processes, with a 5.8% increase in desired care. Heterogeneity exists among studies, and some report more substantial improvements. CDSS interventions have limited impact on clinical endpoints, with a median increase of 0.3% in patients achieving guideline-based targets. Factors influencing substantial improvements remain unclear.
Research has identified errors in electronic medication systems, such as auto-population leading to incorrect documentation and automatic scheduling, causing delays in administration. The lesson is to prioritize system design for better decision-making. Clinical decision support (CDS) is powerful but only resulted in a modest 5.8% increase in desired care, as alert fatigue led to high override rates. Like nudge interventions, behavioural economics frameworks offer subtle ways to improve decision support. Default prescriptions and auto-stop features in critical care units showed positive results in improving care and reducing errors.
In a Canadian [1] coronary care unit, electronic medication systems reduced unnecessary TSH test orders to 0% by removing the option from the standard admission order set. A simulation study showed that organizing antibiotic options influenced prescribers’ choices. Listing narrower-spectrum antibiotics first decreased the selection of broader-spectrum antibiotics from 53% to 30%. To maximize medication safety, thoughtful design and continuous attention are crucial. Monitoring and evaluating changes like altering defaults or introducing new order sets are essential. Addressing technology-related errors and considering non-interruptive alerts are vital in decision support design. Involving end-users throughout the process ensures effective implementation the studies in this section need referencing?
Study 11: “Appropriateness of Overridden Alerts in Computerized Physician Order Entry: Systematic Review” High alert override rates in clinical decision support systems (CDSS) pose challenges to patient safety.
A systematic review of 23 articles found average override alerts ranged from 46.2% to 96.2%, with variable appropriateness. Optimizing alert types and reducing alert fatigue are essential to prevent inappropriate overrides and enhance patient care.
Study 12: “Effectiveness of non-interruptive nudge interventions in electronic health records to improve the delivery of care in hospitals: a systematic review” The study found that implementing nudges in electronic health records (EHRs) can improve inpatient care delivery without interruptive alerts. Approximately 79.2% of the interventions resulted in improved care. However, careful consideration of the sociotechnical system is essential for their effectiveness.
Health Innovation Series
The Health Innovation Series on eMedication Safety aims to provide system managers and users with evidence-based system optimization and user tips in a short format. All issues can be accessed here: https://www.mq.edu.au/research/research-centres-groups-and-facilities/healthy-people/centres/australian-institute-of-health-innovation/our-projects/Health-Innovation-Series/health-innovation-series-e-medication-safety.
Conclusion
Electronic medication systems hold great potential for improving patient safety and healthcare quality. However, to fully realize their benefits, careful attention must be given to system design, addressing technology-related errors, and optimizing clinical decision support. Tailoring systems to specific contexts, involving end-users in the design process, and continuous monitoring and evaluation are crucial steps in enhancing the effectiveness and safety of electronic medication systems.
References
- Braithwaite, J., Glasziou, P., & Westbrook, J. (2020). BMC medicine, 18, 1-8.
- Jha, A. K. (2011).Jama, 306(8), 880-881.
- Westbrook, J. I., Li, et al. (2022). npj Digital Medicine, 5(1), 179.
- Westbrook, J. I., et al. (2012). PLoS medicine, 9(1), e1001164.
- Ash, J. S., Berg, M., & Coiera, E. (2004). Journal of the American Medical Informatics Association, 11(2), 104-112.
- Korb-Savoldelli, V., Boussadi, A., Durieux, P., & Sabatier, B. (2018).IJMI, 111, 112-122.
- Kinlay, M., et al. (2021). RSAP, 17(9), 1546-1552.
- Westbrook, J. I., et al. (2013). JAMIA 20(6), 1159-1167.
- Lyell, D., Magrabi, F., Raban, M. Z., Pont, L. G., Baysari, M. T., Day, R. O., & Coiera, E. (2017). BMC medical informatics and decision making, 17, 1-10.
- Kwan, J. L., et al. (2020). Bmj, 370.
- Poly, T. N., et al. (2020). JMIR medical informatics, 8(7), e15653.
- Raban, M. Z., et al. (2023).JAMIA 30(7), 1313-1322.
Author
-

Senior Research Fellow, Australian Institute of Health Innovation, Macquarie University



