A Quality Improvement Collaborative for a long COVID: Building the boat as we sailed it
Read the Magazine in PDF
Abstract
The Quality Improvement Collaborative for Long COVID aims to improve outcomes and quality of life for long COVID patients. It utilizes the C19 YRS rehabilitation scale to measure symptom severity for tailored treatments. The collaborative seeks to develop guidelines for long COVID assessment and management in primary care, addressing referral pathways and patient involvement to enhance care. Recent research findings emphasize accurate diagnosis and coding in primary care to provide appropriate care and support for long COVID patients in the future.
Introduction
Continuous quality improvement in healthcare involves data analysis and changes to enhance patient outcomes. The “Building the Boat as We Sailed it” approach draws from Otto Neurath’s analogy to navigate the evolving challenges of long COVID. The Quality Improvement Collaborative for Long COVID was established to gather data and improve clinical practices collaboratively with patients and healthcare staff in response to the multi-system disease caused by COVID-19.
What is long COVID?
Long COVID refers to the persistent symptoms and complications that some patients experience after recovering from the acute phase of COVID-19. These symptoms are as follows; Fatigue Pain Brain fog to various neurological issues.
What is the prognosis of long COVID?
Around 1 in 3 covid-19 patients still have symptoms 4 weeks after the acute illness Half of these will be symptom-free by 12 weeks (~1 in 10 still troubled) Half of these will be symptom-free by 6 months (~1 in 20 join the ‘tail’ of covid long haulers)
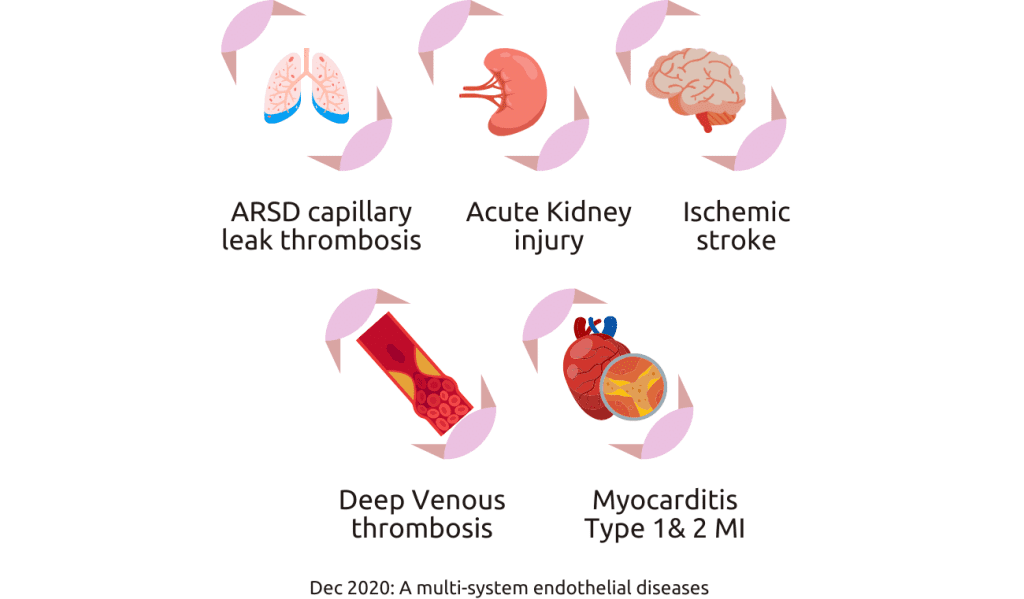
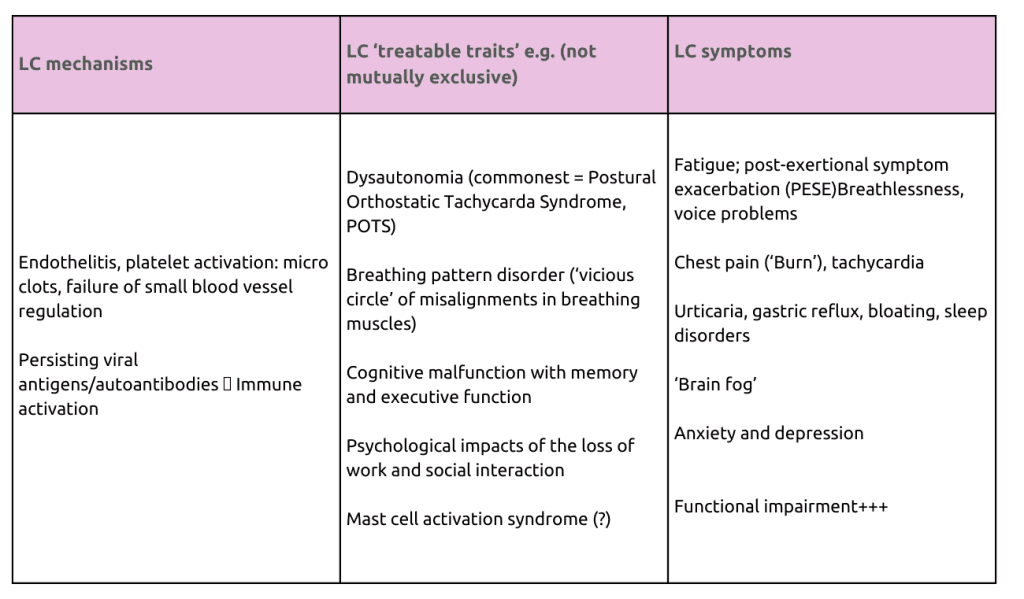
Long COVID is a post-viral syndrome causing various symptoms like fatigue, cognitive issues, anxiety, and chest discomfort. Its exact mechanisms involve inflammation and damage to the body’s systems. Seek medical help if experiencing these symptoms. There are a number of resources available to help people with COVID, including;
- The Long COVID Clinic
- The Long COVID Coalition
- The Long COVID Forum
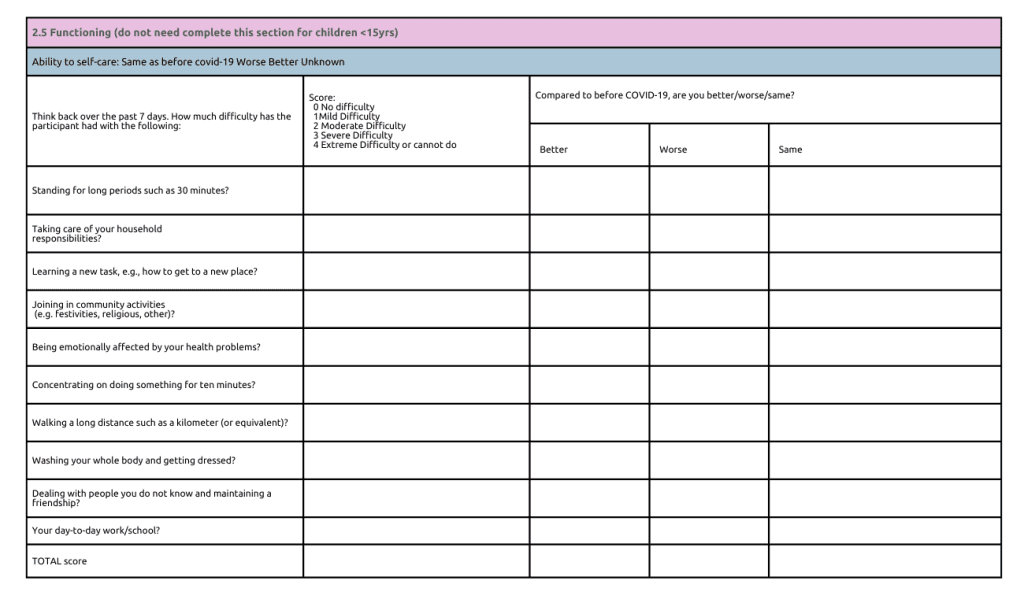
According to the World Health Organization’s evaluation form, functional impairment is a crucial factor in diagnosing long COVID, as patients may struggle with basic activities like dressing, washing, and socializing.
Recognizing and diagnosing long COVID is challenging, particularly in countries like India.
Long COVID: A tiered approach
The UK’s tiered approach, with specialized clinics, has shown success in managing patients. Accurate recognition and diagnosis are vital for effective management, necessitating communication and coordination between tiers.
The tiered approach works as follows:
- Tier 1 provides support for self-management
- Tier 2 provides primary care
- Tier 3 has specialized teams helping patients manage symptoms
- Tier 4 care is necessary for patients with specific complications.
It is essential to have a comprehensive approach to managing long COVID patients to provide the necessary care and support.
Long COVID: Which paradigm?
It is important to have a comprehensive approach to managing long COVID patients. There are three different approaches to addressing long COVID.
- Biomedical paradigm: Finding drugs to alleviate symptoms.
- Rehabilitation paradigm: Gradually increasing physical activity while emphasizing self-pacing to avoid negative effects.
- Relationship-based care paradigm: Strong connections between patients and caregivers.
LOCOMOTION: Quality improvement collaborative
- NIHR funded 9 sites in England to improve long COVID care, with the main site in Leeds and 8 others nationwide.
- The team uses the “potentially better practices” approach based on feedback from participating sites, prioritizing quality improvement over RCT evidence.
- NIHR funded 9 sites in England to improve long COVID care, with the main site in Leeds and 8 others nationwide.
- The team uses the “potentially better practices” approach based on feedback from participating sites, prioritizing quality improvement over RCT evidence.
- While RCTs are conducted elsewhere, their focus is on enhancing clinics using rapid cycle testing of change.
- Some aspects lack trial data, prompting clinicians to learn from practice and improve care quality.
Should we standardize outcome measures within and across clinics?
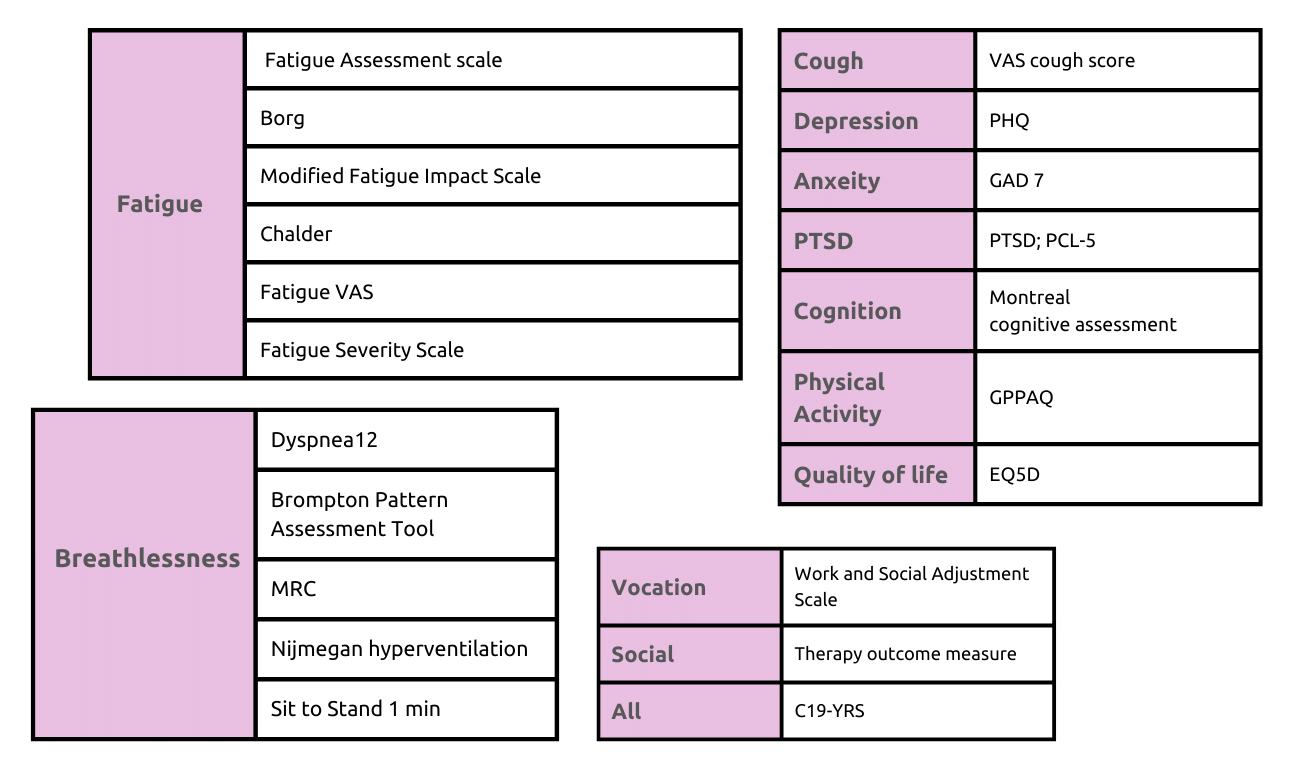
A study identified various outcome measures used by clinics for assessing PTSD and long COVID recovery. To standardize evaluation and data collection, a new measure called C19-YRS was developed, covering physical, psychological, and social aspects. It has proven reliable and valid.
C19-YRS
The C19 YRS rehabilitation scale is a patient-reported outcome measure designed to assess the severity of long COVID symptoms. It covers all long COVID symptoms, categorizing each as mild, moderate, or severe, providing a comprehensive evaluation of all ten organ systems.
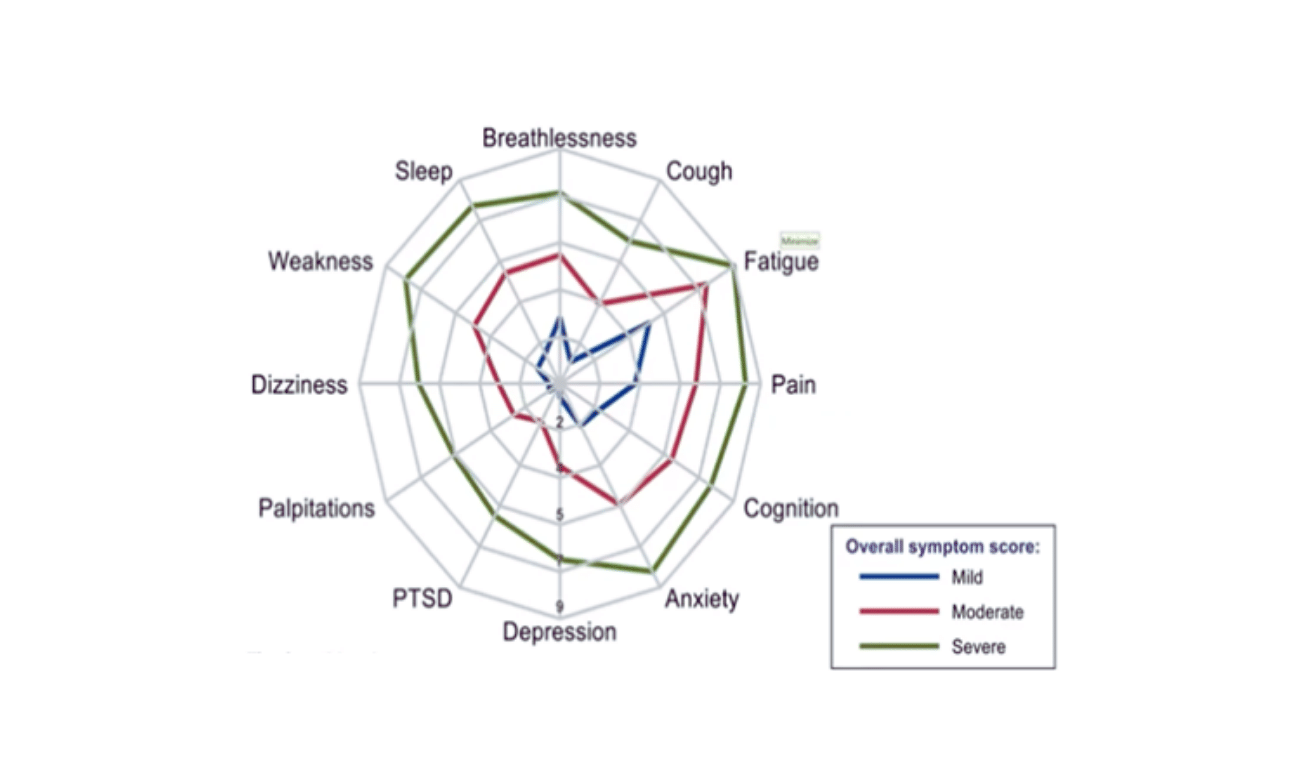
The C19 YRS rehabilitation scale has several benefits, including:
- Personalized treatment plans by healthcare professionals.
- Changes in symptoms are continuously monitored over time
- A graphical display of the changes in the patient’s symptoms over time.
However, some clinics do not use the C19 YRS rehabilitation scale because the Patient pathways can be varied, which requires the use of different outcome measures and there are differing opinions among healthcare professionals about its effectiveness.
What investigations and initial management should people have when seen in the specialist clinic?
When seen in the specialist clinic, individuals with long COVID should undergo a thorough assessment, including a review of their medical history and a physical examination. Initial management involves offering reassurance and support, with possible referral to specialty clinics if needed. Healthcare professionals should coordinate care, stay updated on the latest evidence, and collaborate with patients to develop a tailored management plan.
Regular monitoring and adjustments to the plan are crucial.
Greenhalgh et al. provide an update on long COVID, discussing possible physician responses to patient queries. Long COVID refers to persistent symptoms after SARS-CoV-2 infection, encompassing “ongoing symptomatic COVID-19” (4-12 weeks), “post-COVID-19 syndrome” (more than 12 weeks), “post-COVID conditions,” and “post-COVID-19 condition” as defined by NICE, CDC, and WHO.
What should be the referral criteria for long COVID clinics?
The referral criteria for long COVID clinics should include individuals who are experiencing persistent or prolonged symptoms after a COVID-19 infection. Common symptoms may include fatigue, breathlessness, cognitive issues, chest pain, and other persistent or recurring health problems related to COVID-19.
The Quality Improvement Collaborative (QIC) has significantly improved extended COVID management in primary care. Guidelines and infographics were developed with patient involvement. The guidelines recommend thorough assessments, reassurance, specialist referrals if needed, coordination with other professionals, and staying updated on evidence. The QIC’s efforts have positively impacted care provision and GP knowledge. Whole-person care, symptomatic management, and vaccinations are crucial. A patient-friendly paper aids understanding, and in India, understanding long COVID presentations helps improve support and referrals in primary care. More research is needed, but QIC’s work benefits extended COVID support.
Quality Improvement Collaborative for Long COVID: Patient experience
The QIC prioritizes patient experience through qualitative research on long COVID’s real-life impact.
Their BMJ Open study explores first-hand experiences of brain fog due to COVID, and they collaborate with neurophysiologists to investigate brain physiology irregularities linked to these experiences.
Study 1: “I can’t cope with multiple inputs”: A UK-wide qualitative study explored the experience of “brain fog” after COVID-19. 50 participants, mostly non-hospitalized women, shared diverse neurocognitive symptoms. The findings call for more research and tailored services for patients with these symptoms.
Study 2: “Long Covid – The illness narratives”: Rushforth et al. analyzed patient narratives from social media, challenging the view of COVID-19 as a short-lived respiratory illness. Patients advocated for better care, influencing guidelines and policy. The study emphasizes the vital role of extended Covid communities in shaping understanding and treatment.
Study 3: “Persistent symptoms after Covid-19”: Ladds et al. investigated 114 “long Covid” patients’ experiences, revealing complex and fluctuating. symptoms. Challenges in accessing diagnosis and care led to feelings of loss and stigma. Proposed quality principles for Long Covid services include accessible care and multidisciplinary rehabilitation.
LOCOMOTION QIC: Reflections
The UK’s Quality Improvement Collaborative (QIC) encounters challenges in implementing initiatives, including financial strains, workforce shortages, and tensions over costly investigations. Philosophical issues arise concerning subjective and objective knowledge and balancing local practicalities with universal truths. Identifying long COVID cases in deprived areas and addressing political and ideological obstacles are concerns. Nevertheless, the QIC remains committed to evidence-based, interdisciplinary efforts to improve long COVID care.

Conclusion
The QIC’s efforts to improve extended COVID care are commendable, despite facing obstacles. Reflections on philosophical, practical, and political aspects have led to addressing health inequalities and unmet needs.
The QIC remains dedicated to evidence-based, interdisciplinary approaches. Continued support and investment in their endeavors are vital to improving the lives of those affected by long COVID.
References
- Greenhalgh, T., Sivan, M., Delaney, B., Evans, R., & Milne, R. (2022). Long covid—an update for primary care. BMJ, 378.
- Callan, C., Ladds, E., Husain, L., Pattinson, K., & Greenhalgh, T. (2022). ‘I can’t cope with multiple inputs’: a qualitative study of the lived experience of ‘brain fog after COVID-19. BMJ open, 12(2), e056366.
- 3. Rushforth, A., Ladds, E., Wieringa, S., Taylor, S., Husain, L., & Greenhalgh, T. (2021). Long covid–the illness narratives.Social science & medicine, 286, 114326.
- Ladds, E., Rushforth, A., Wieringa, S., Taylor, S., Rayner, C., Husain, L., & Greenhalgh, T. (2020). Persistent symptoms after Covid-19: a qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC health services research, 20(1), 1-13.





