Improving Patient Transitions from Hospital to Home: A Quality Improvement Project
Read the Magazine in PDF
Abstract :
This article presents a quality improvement project initiated by Fortis Healthcare Limited, Chennai, to enhance planned discharges. The project aimed to improve the coordination of patient transitions from the hospital to home by developing personalized discharge plans. The team conducted a five-point analysis to diagnose the problem and found the root cause was the lack of a structured discharge planning and communication approach. The hospital implemented various solutions, including establishing a transparent process with defined responsibilities and timelines for planned discharges, drafting patient updates, and updating bills. The project resulted in significant improvements in planned releases; patient experience scores with the discharge process, and discharge complaints. The intangible benefits included increased consultant involvement, better stakeholder communication, and a streamlined admissions process.
Organization Profile
Fortis Healthcare Limited, a subsidiary of IHH Healthcare Berhad, is a leading healthcare services provider in India with a presence in the United Arab Emirates and Sri Lanka. The company operates 27 healthcare facilities with over 4,100 operational beds and 419 diagnostic centres. With a partnership with IHH, Fortis aims to become the world’s most trusted healthcare network. Fortis Hospital in Vadapalani is the second facility in Chennai, offering personalized care to cater to each patient’s unique needs. The 250-bed multi-speciality hospital features state-of-the-art facilities, including a centre of excellence in Cardiac, Gastro, Liver and HPB, Renal, Neuro Sciences, Trauma and Orthopedics Care. The hospital has the largest multi-organ transplant centre in Chennai, including the heart, lung, liver, kidney, small bowel, and pancreas.
Introduction
Enhancing planned discharges is a project initiated by the Medical Administration Head and PCS Team at this hospital. The project aims to improve the coordination of patient transitions from hospital to home by developing personalized discharge plans. Due to the hospital being newly established in 2020 and the presence of multiple consultants from different institutions, not all medical team members were following the process of planned discharge. The project aims to involve patients and families in the process, avoid complications, and enhance efficiency. Moreover, the patients and their families have provided feedback regarding the delay in the discharge process and the lack of information about expected discharge times. A well-coordinated approach to discharge, including planned releases and a seamless transition, can help improve the patient experience and prevent delays in the discharge process.
Furthermore, the team conducted a five-point analysis to determine the underlying cause of the problem. The analysis revealed the following root causes:
- The reason for the discharge process not being planned: The consultants did not follow a structured approach for designing the discharge of admitted patients.
- The consultants failed to follow a structured approach for discharge planning: The hospital had multiple consultants, including visiting consultants from diverse backgrounds with different work styles, resulting in a lack of structured discharge planning.
- A lack of structured discharge planning: There is no clearly defined mechanism for timely communication and planned discharge initiation.
- A defined mechanism is not being implemented for discharge planning: The lack of clarity in information flow and role identification has resulted in the absence of a structured approach.
- A lack of clarity in information flow and role identification: The process was not clearly defined and communicated to all stakeholders involved in the discharge planning process.
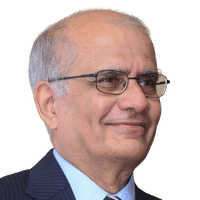
The following goal statements were created in response to the defined problems:
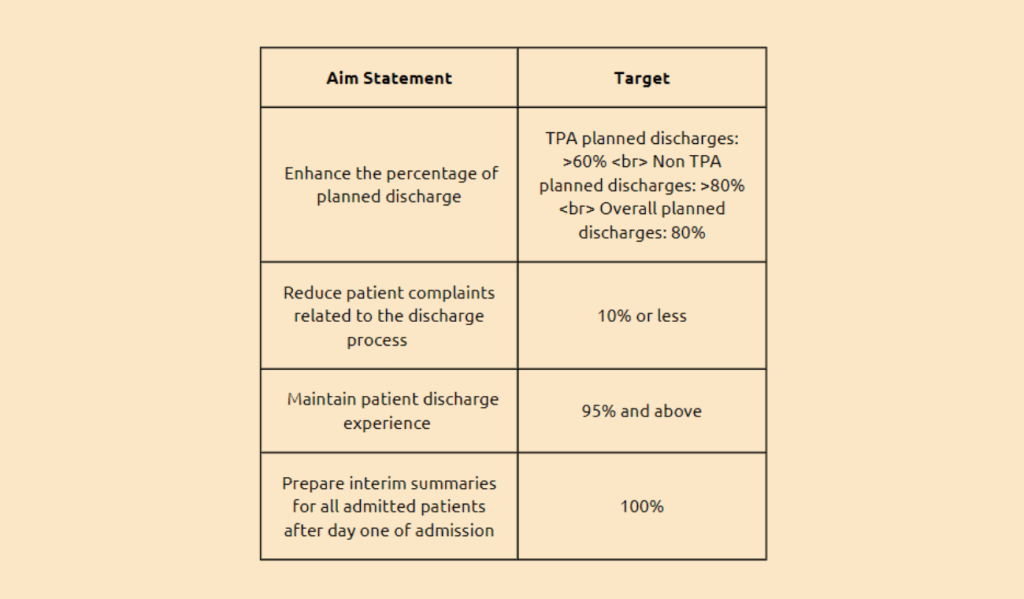
Outcome:
Planned discharges were enhanced by:
- Improve planned discharges by establishing a straightforward process with defined responsibilities and timelines.
- Ensure all consultants know the importance of planning tentative discharge dates at the time of admission.
- Have the MODs share the list of planned discharges for the day in the WhatsApp group before 11 AM.
- Instruct the Duty Medical Officers to prepare the patient’s summary draft.
- Assign a D/C summary clerk in the wards to update the patient’s condition in the summary draft.
- Ensure that bills, including procedure charges, are updated daily on the same day.
- For non-cash patients, send interim summaries and bills to TPAs.
- Send bills and summaries to patients one evening before discharge.
Provide patient counselling on the discharge procedure by the PCS team.
Expected outcomes from the plan include:
- Clear and structured communication of planned discharges to duty medical officers and nurses.
- Prompt initiation of the discharge process by the MOD and PCS team.
- Availability of readily-drafted patient updates from the date of admission or procedure.
- Daily updating of bills to keep patients informed of expected costs.
- Improved patient satisfaction through a reduction in complaints related to the discharge process.
Implementing the quality improvement project involved several effective methods to enhance the planned discharge process. To ensure smooth and efficient discharges, treating consultants were actively engaged, providing their expertise and input to optimize the discharge planning process.
Daily draft summaries were also prepared with the involvement of the Duty Medical Officer (DMO) and secretaries, facilitating better coordination and communication among the healthcare team. Immediate post-procedure billing updating was also implemented to streamline financial processes and minimize delays.
To ensure the sustainability of these improvements, ongoing monitoring of planned discharges is being carried out. This monitoring process helps identify potential issues or areas for further improvement, allowing for timely interventions and adjustments. By consistently monitoring the planned discharges, the healthcare facility can ensure the continued effectiveness of the implemented strategies and maintain a high standard of patient care.
The initial study conducted in 2021 focused specifically on surgical discharge patients, aiming to improve the discharge process for this particular group. However, the success of the improvement measures prompted their extension to all ward-admitted patients. By replicating the established improvement strategies, the benefits observed in the surgical discharge process can now be realized across the entire facility, ensuring a more streamlined and efficient discharge process for all patients.
A proactive approach was adopted to address any issues related to unplanned discharges. Any instances of unexpected releases are immediately escalated to the medical head, allowing for prompt assessment and appropriate action. By addressing these incidental discharges promptly, the healthcare facility can minimize potential adverse outcomes and ensure patient safety.
Additionally, daily discharges are regularly analyzed to monitor the effectiveness of the implemented improvement measures. This analysis allows the healthcare team to evaluate the impact of the improvements, identify any areas for further refinement, and make data-driven decisions to optimize the discharge process continually.
By extending the improvement measures beyond the initial study and implementing them across different patient populations, the healthcare facility can ensure consistent and standardized care, enhance patient satisfaction, and promote efficient and effective utilization of resources
Conclusion :
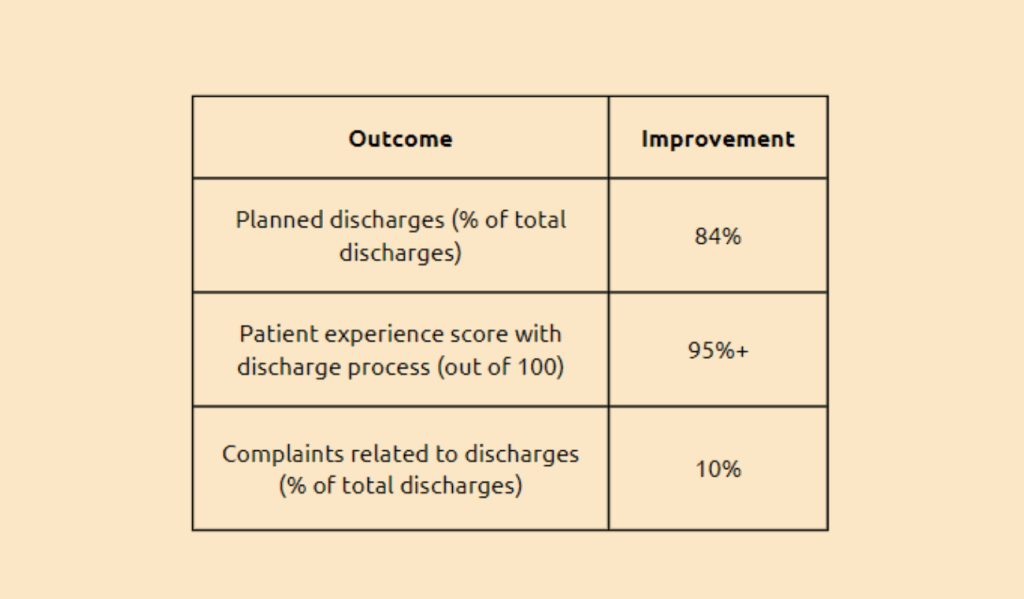
The “Enhancing Planned Discharges” project at Fortis Healthcare Limited in Chennai successfully implemented measures to improve the coordination of patient transitions from hospital to home through personalized discharge plans. The project addressed underlying problems such as the lack of structured discharge planning, poor communication, and delayed discharges. Implementing a straightforward process with defined responsibilities, improved communication, and daily monitoring resulted in tangible and intangible improvements, such as a higher percentage of planned discharges, increased consultant involvement, and a streamlined admission process.