Improving medication safety in the modern era
Read as Magazine PDF
OUTLINE
- What we know about improving medication safety:
- CPOE
- Decision Support
- Bar Coding
- Medication reconciliation & EHR
- Smart Pumps
- CPOE
- Potential for Harm/Pitfalls
- Current State
THE IMPORTANCE OF MEDICATION SAFETY
- Drugs are one of the biggest causes of harm to healthcare
- In inpatients, opiates are a major cause of leading to 20% of ADEs
- Substantial harm in OP settings as well
Medication errors are common, but most of them have little or no potential for harm. A small proportion of the potential adverse drug events do have the potential to harm a patient, but most of those do not harm patients. The ones that we’re the most concerned about is, is the preventable adverse drug events, which are the errors that do harm someone. And even most things that do harm someone or are not preventable. According to a study we did on 10,070 orders, we realized about one in 100 medication errors result in an adverse drug event and seven in 100 have the potential to do so.
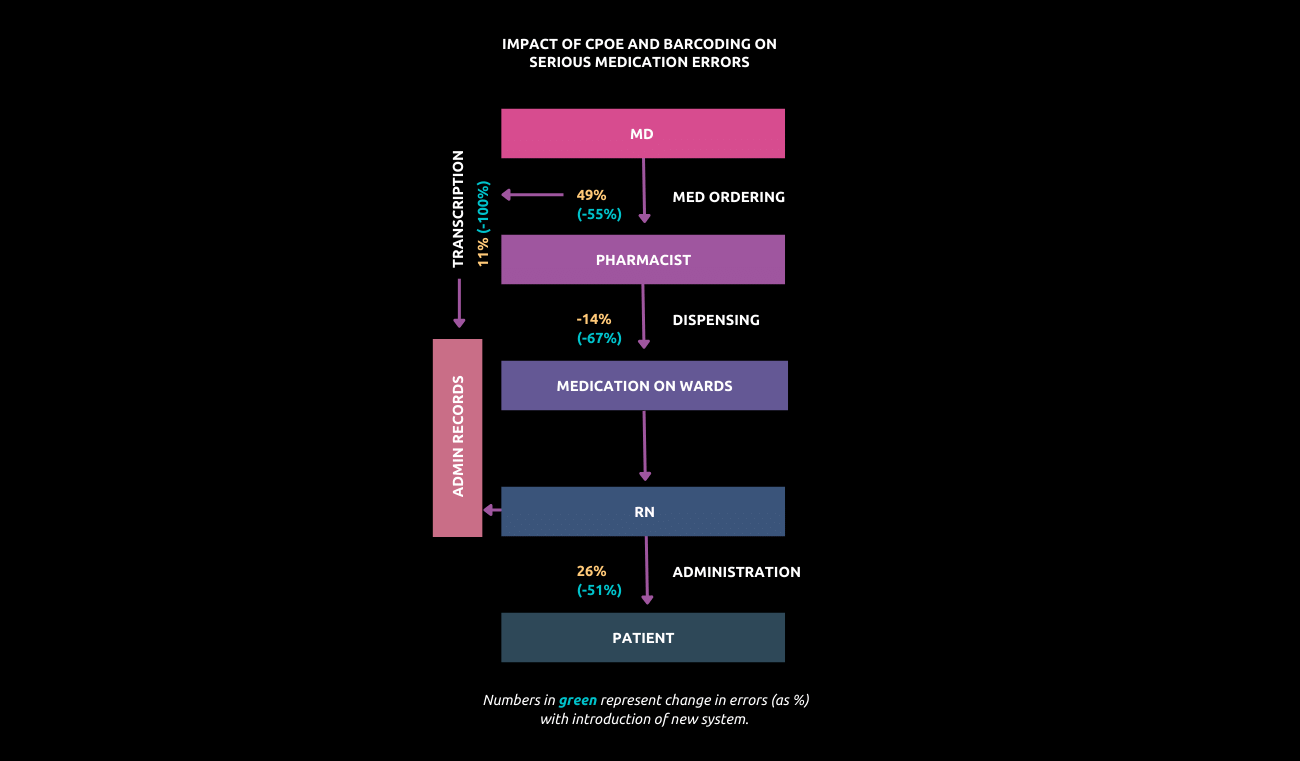
The key findings of that study were that there were six and a half adverse drug events for every 100 admissions. 28% or about a third were preventable. There were three potential adverse drug events for every preventable adverse drug event and 62% of the areas wherein the ordering and transcription stages. And that was a bit of a surprise because many of the studies to that point had assumed that ordering was done by physicians and then it was always done correctly. What this showed was that that was not the case. We also looked at the cost of these events and showed that they’re expensive and they cost nearly USD 2500 at that time for adverse drug events and even more for preventable events.
Another study was done in another state Utah, and they reached an estimate that was about the same as ours. We estimated that just at our hospital, the cost for all adverse drug events was $5.6 million a year and roughly half of that was preventable. And that didn’t include any of the costs of injuries to patients, didn’t include malpractice costs or the cost of admissions due to adverse events. This is the kind of thing that we’ve been able to use to justify prevention efforts. So if if you think about the process, there are several things that you can do to improve its safety first.
Computerized order entry
Other things that are really important include barcoding, smart pumps, computerized monitoring for adverse drug events, and having a pharmacist contact patients after they go home because patients often suffer problems after they go home. A couple of reviews have looked at computer order entry and medication safety, and they’ve confirmed that it’s a powerful tool for improving safety. One study suggested a 66% reduction in prescribing errors on average. In another study that looked at both order entry and adverse drug events in five of ten studies, five showed a decrease in the adverse drug event rate. Four showed nonsignificant trends. One showed no effect. That’s about what you’d expect because most of these were not powered to detect a difference in the frequency of adverse drug events. The rules that we use are often, often not as good as they should be.
In most of the systems, even when you display an alert, most of those alerts get overridden. And what we did was to go through and turn off a lot of the unimportant ones. And we found that over six months, we had 1800 18,000 alerts, and roughly 71% were non-interrupted. So that means they appeared on some part of the screen, but the physician didn’t need to do anything. 29% were interrupted. And of the interactive alerts, 67% were accepted. We’re not at that level of performance now. We’re often just displaying alerts to the physicians like crazy and they’re overwriting nearly all of them. And that’s not very helpful for improving medication safety.
We showed early on that tier-ing was important for improving the rate at which people respond to events on Inpatient DDI alerts.
So here we studied two academic centres. They used the same knowledge base that says they used three tiers. The top tier was a “Stop”. You can’t proceed. The next here was, “We think you should do something different”. And then Tier three was, “We’re going to make you aware of it, but you don’t have to do anything differently”. We had all the alerts interruptive or level two. And what we found was that it’s safe to say that 100% of the time people stopped when they got one of the most severe warnings versus only 34% at the monitor site. So that means 66% of the time people were running the stop sign and the overall alert acceptance rate was also higher at the site, 29% versus 10%.
We also figured out which drug interactions are the most important. And here what we found was that there were just 15 drug class pairs that were important. And basically, you should never get those drugs together. They’re candidates for stop alert.
We weren’t sure that this is the absolute complete set of these, but these were the pairs that our experts agreed about. And I do want to underscore that the less significant drug interactions are still important. They’re much more prevalent. They probably cause much more harm. That’s things like warfarin and self-addressed, which, you know, it’s the sort of thing that is given all the time. It tends to depend on patient characteristics like drug doses and timing and common conditions like hyperkalemia. And to improve the sensitivity and specificity of these, we need more investment and evidence for the generation and then methods for making drug interactions conditional on patient data.
SIMULATIONS
One of the things that we’ve done that we’re excited about in the U.S. Is to develop a tool, which is essentially a flight simulator for computer order entry in which our hospitals take orders and put them into a computer system with it with test patients. And you can then check and see how well your system is working.
SAFETY RESULTS OF CPOE DECISION SUPPORT
- 62 Hospitals voluntarily participated
- Simulation detection only 53% of orders which would have been fatal
- Detected only 10-82% of orders which would have caused serious ADEs
- Almost no relationship with vendors
And when we started this, we got 62 hospitals around the country to voluntarily participate. And we found that the simulation detected only 53% of the orders which had killed someone. So really not a very good performance. And it detected only between ten and 82% of orders, which would have caused serious adverse drug events. Notably, there was almost no relationship with the vendor. People have the feeling that if they bought the right vendor, their system would be safe. This shows that was not the case.



Each hospital has a lot of ability to tune its system, turn the warnings on, or turn them off. And the performance that you got depended on where you had set that. Notably, most of the institutions had no insight as to where they were on this spectrum. And over time, we’ve done more with this with another study that we did showed that the better you do on this particular test, the better your safety is. So there was a 43% reduction in your medication error rate for every 5% increase in the Leapfrog score. And we’re also for fewer preventable adverse drug events for every 100 admissions for a 5% increase in your score. So if you do better on this, you deliver safer care. And over time, the number of hospitals taking the test has gone up a lot. We have about 5000 hospitals in the US and we now have close to 2000 taking the test on an annual basis and the average per cent correct has gone up a bit. But we keep making the test a little bit harder. And hospitals continue to learn, even if they’ve taken the test every year. And I think this kind of post-implementation testing is a really useful thing going forward.
SMART PUMPS
Another technology, which is that is potentially really helpful for improving medication safety is smart pumps. These are pumps that can be told what drug is being given so that there can be a check put in place to make sure that the dosage that the patient is getting is correct. And we did a study on this early on and showed that serious IV Medication Errors were frequent and we could detect them using smartphones. However, we found no impact on the serious medication error rate or the preventable adverse drug event rate. And that was almost certainly because of poor compliance on the part of nurses suggesting that both behavioural and technological factors have to be addressed for smartphones to achieve their potential for improving medication safety. We did this work directly with a vendor, and they then went through and changed their application to make it much safer.
Another type of there that can be tragic is putting the wrong medication into a medication cart. We had a case in Indiana in which three babies died as a result of having adult-strength heparin put into the cards that were going to neonatal care units. And this is something that if it’s administered, it’s usually fatal. The first baby died. They weren’t able to figure out what was going on. The second baby died. So there was confusion in that until the third baby died.
BARCODING & DISPENSING SOLUTIONS
Barcoding we use in supermarkets, for example, all the time. We should be using it in health care, too. A study that we did that was led by Dr Kern that looks at the dispensing error rate after you put in place barcoding and the dispensing error rate fell substantially by 31%. The potential of that rate fell even more, 63%. And we did a formal cost-benefit analysis of this that showed that the five-year cumulative costs were 2.3 million, but the five-year cumulative benefits were five and a half million. So and the break-even was within the first year of the goal line. So not only does this improve safety, but it’s that it’s cost-effective. We also then looked at the impact of putting barcoding in place at the bid site, and this is the place where it probably has the biggest impact. And this is a study that was published in the New England Journal.
And we showed the medication error rate fell by 41%. If you put in place barcoding and the potential adverse drug event rate fell by 51%. And this has resulted in barcoding being nearly universally adopted. Now in that in the US it’s been made a safe practice and it’s expected that you have barcoding and medications in place and at your institution.
POST-DISCHARGE INTERVENTIONS
Another thing, which is pretty simple but can also make a big difference is intervening post-discharge. This is work that was led by Dr Jeff Schnipper here. We did a trial of having a pharmacist call patients 3 to 5 days after they’re admitted. And what we showed was the preventable adverse event rate incidence was just 1% in the intervention group versus 11% in the control group. Now the problem in getting this implemented in the U.S. is that our insurance doesn’t pay for it in most states. But this is something that improves safety.
INPATIENT SOLUTIONS
So if you look at the inpatient profile overall, there are many different pieces. I think computerizing ordering is the most important one, but barcoding is important to this point of care technology. So a smart pharmacy was doing better with medication reconciliation in the U.S. still today, many of these don’t communicate with each other. They should. And we also need to monitor for medication errors and events and spontaneous reporting.
SOME STUDIES PAINT ONLY A PARTIAL PICTURE
One was a study that was done at the University of Pittsburgh Pediatrics looking at computer order entry. They studied children who are being transported for special care. And the authors of this study that was published in Pediatrics showed that the mortality rate went up from 2.8% to 6.3%. So, an odds ratio of 3.3 after a complete commercial computer order entry application was introduced. Now, the study design was before or after. Other changes were made. At the same time, a computer order entry was implemented and they didn’t report the overall mortality rate, which is a little surprising. But when you dig deeper into this and you put on your quality and safety hat, you know, you find several important things. First of all, it introduced computer order entry very rapidly over six days, which is probably too fast for that big change. After the implementation, order entry wasn’t allowed until the patient had entered the hospital and had been logged into the system. And the kids that they were studying were kids who came in often in a helicopter or certainly in an ambulance. And in the past, many of the orders have been written while the patient was still on the way. So by the time the child got to the institution, everything could be ready for them. After the computer and the implementation of the study, all the drugs were moved to the central pharmacy, which was very far away from intensive care. A rule was put in place that the pharmacy couldn’t process medication orders until after they were activated. Many of the order sensor groups of orders weren’t available initially, and this turns out to be a huge deal because it’s faster to write orders than on the computer, but it’s a lot slower to write individual orders. And then that result here was substantial delays for delivery. And it’s possible that this introduction did, in fact, cause these problems. Now, this study was quite
weak methodologically. It was before or after. But the increase in the mortality rate, with large and obvious concerns and introducing these big delays in the group, could have cost us this problem. But if you dig deeper, many of the rules for implementation were not followed, and it’s just essential for other organizations to handle these socio-technical aspects better.
There have been other studies that looked at the same question. Another study at the University of Washington and their pediatric intensive care unit looked at a before and after implementation of order entry and it was actually exactly the same commercial order entry system where they showed that their mortality rate actually fell in another study that was done in another institution, Montefiore, showed the same thing that their rates, their rates fell. So almost certainly this was related to how things were implemented in Pittsburgh. And I think that’s a powerful message in terms of quality and safety.
WHAT HAS CHANGED
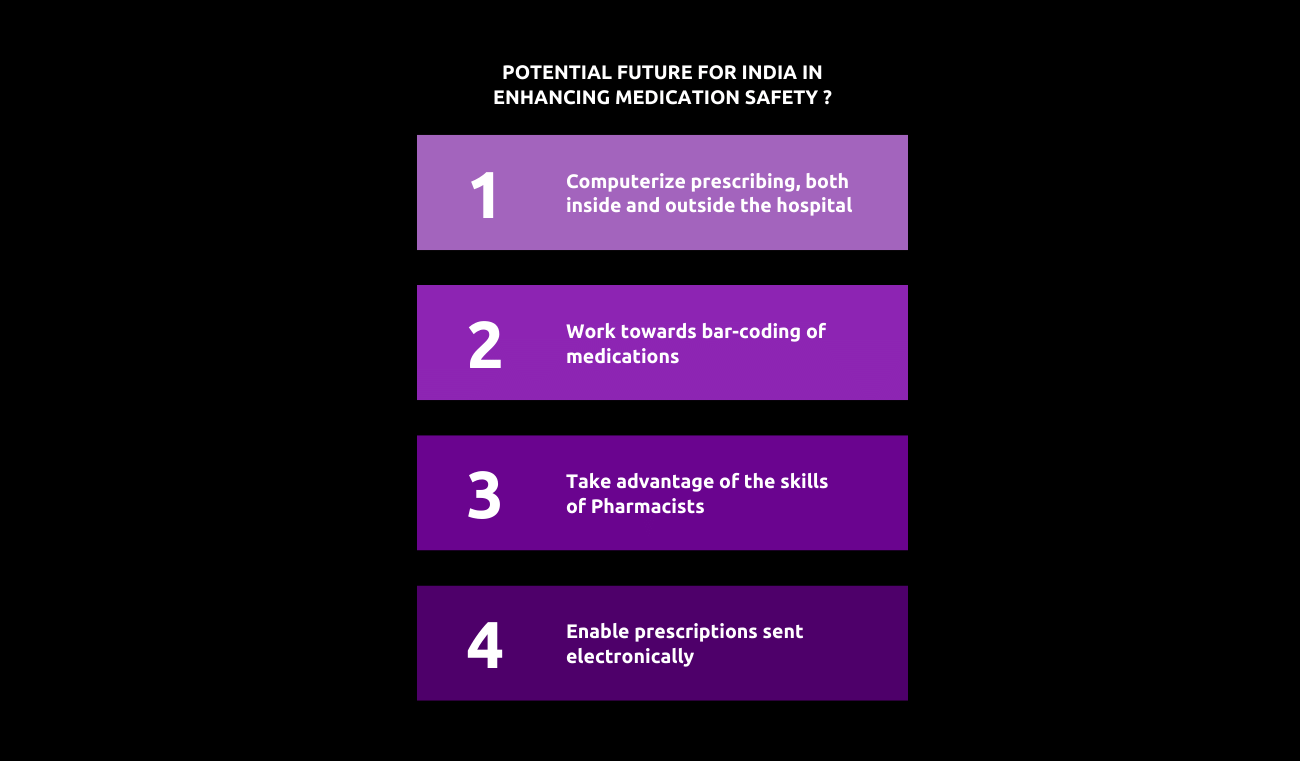
We now in the US have really universal use of electronic health records in the patient in the outpatient setting. That’s increasingly true in other developed countries and most parts of Europe, for example, there’s universal use in the outpatient setting, but not necessarily in the patient setting. There’s computerized prescribing and the US prescriptions go electronically, directly to pharmacies, which is a big win. But there are still problems.
In particular, clinical decision support is not yet delivered around medication safety. And I’ll tell you some more about that in a bit. Prescriptions often still are not received in coded form, which is a problem. Here’s the study that was led by Dr Adrian Wong that was published in 2018. And we looked at decision support overrides in the intensive care unit. We looked at six cases and identified 2448 overwritten alerts. The doctors were appropriate to override 81% of the time. There were more adverse drug events found after inappropriate overrides, as you’d expect, 16 and a half versus 2.7 now. And the implication there is we have to do better with our decision support in terms of positive predictive value.
But here’s an even more troubling study that we did recently. The study was led by Dr Adam Wright. We looked at drug interactions after conversion to a commercial electronic record, the overall alert burden, and the rate at which people saw it increased by six. The acceptance rate for the most severe warnings fell from 100%, as you were not allowed to override before, to 8.4%. So people, even for the things that you should basically never give a patient, were overriding 92% of the time and the override rate fell from 29.3% to seven and a half per cent for medium warnings. The institution did then disable the least severe alerts, which dropped the warning rate by about half. But the acceptance rate for the most severe only increased from 9.1 to 12.7%. So that’s still an abysmal performance. The implication is we have to refine the underlying decision support and turn off more of the false positives.
There are a number of things that are going on on the technical front. So there are new sensors that can detect what medication is in the solution and at what concentration of pumps can be wirelessly updated so that you don’t have to do a lot of programming with them. There can be seamless linkages between centralized systems and delivery devices. Monitoring can be used in many locations, including the home. We’ve done some studies on contact list monitoring in which you have a device that goes between the mattress and the bed. So it never touches the patient and it can monitor things like respiratory rate and pulse very accurately big data techniques and artificial intelligence are likely to be increasingly important.
What will it take to transform care?
INPATIENTS
- The key issue is to make essential processes more reliable
- New approaches like CPOE, bar-coding etc.
- Linking these approaches
- Using clinical pharmacists to the best advantage
- Measuring performance
OUTPATIENTS
- Computerized prescribing, strong decision support
- Addressing adherence issues
- Using clinical pharmacists to the best advantage
- Monitoring patients better
ALL SETTINGS
- Leveraging data to personalize for patient
Author
-

Chief, General Internal Medicine, Brigham and Women's Hospital, Harvard Medical



