Why do we need Patient-Reported Experience Measures (PREMs)?
Read the Magazine in PDF
Introduction
17th September 2023 marks a landmark day in patient safety and healthcare quality history. This is World Patient Safety Day, and the World Health Organisation (WHO) has declared the theme “Engaging patients for patient safety” with the slogan “Elevate the voice of patients”. There are various means of involving patients in patient safety. Still, we believe that when we think of the effectiveness of these measures and their impact, no other measure can come even closer to patient-reported experience measures (PREMs). This whitepaper explores different ways of implementing PREMs, various uses of PREMs, and their limitations with experiences of implementing PREMs.
Merely talking about patient involvement in care is simply not good enough and we need to establish a clear picture of what happens during each care episode.
Patient-reported experience measures (PREMs) are a critically important tool to ensure that the patient safety policies and protocols are being implemented by our healthcare workers and thereby ensuring patient safety. If used effectively, these tools can provide plenty of benefits. These are discussed in this whitepaper along with offering simple tricks to implement PREMs at your facility.
Why do we need PREMs?
Patient-centred care has become the buzzword in the healthcare industry over the last two decades, with a plethora of initiatives, protocols, and processes being introduced to ensure patient safety as well as patient and family satisfaction.
Worryingly enough, despite all these measures, we continue to encounter an alarmingly high number of incidents of patient harm in our healthcare facilities. Mehtsun, Ibrahim, and Diener-west 2013 reported 4082 surgical never events in the USA [1]. NHS alone, reported as many as 368 serious and avoidable ‘never events’ between 1st April 2021 to 28th Feb 20222, as shown in figure 1.
Events such as performing surgery on the wrong part of the body, leaving foreign objects inside the body, or using the wrong implants and/or prostheses are unfathomable in the modern world, but as the report suggests, these events are a regular occurrence in a developed healthcare system like NHS.
As per some estimates the NHS in the UK has around 108,000 patient beds as compared to 757,000 beds in India. Most of the NHS and USA facilities are already implementing various patient safety protocols whereas we in India still have a lot of scope for improvement. Considering these factors we can imagine the extent of the problem in the Indian context.
These astonishingly high numbers clearly establish the fact that the current measures being implemented by healthcare providers are not enough to safeguard our patients.
Since most of the healthcare facilities in NHS follow safety protocols and NHS still reports more than one ‘never event’ happening in NHS every day, we can imagine the number of such horrible accidents happening in the less developed parts of the world.
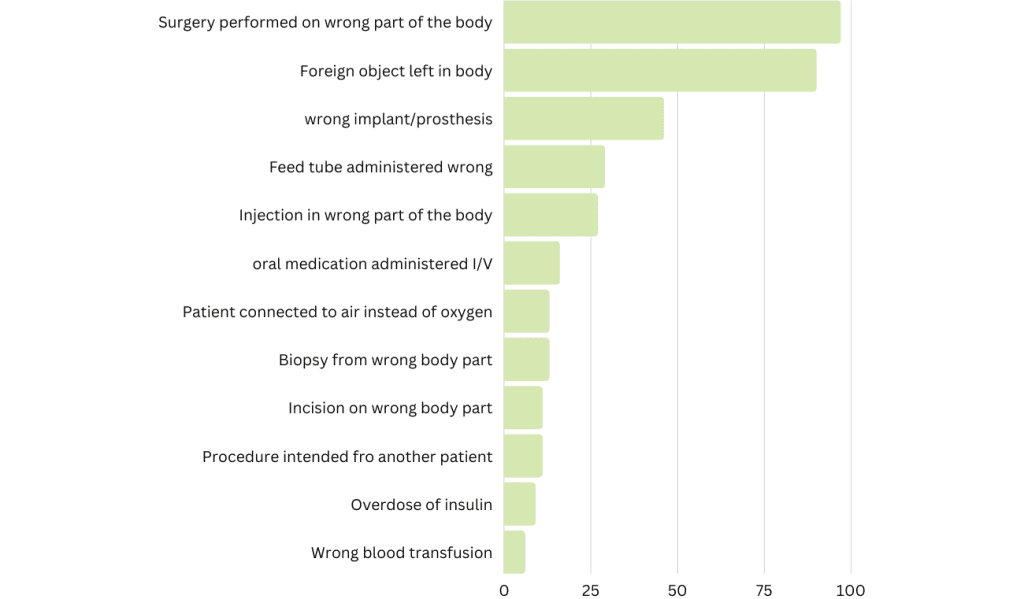
Figure 1: The NHS’s most serious (and avoidable) errors of 2021. Several serious medical errors occurred in England despite being wholly preventable (April 2021- Feb 2022). Source: National Health Services (NHS).
The healthcare industry has been developing various protocols and guidelines to prevent such horrific accidents but despite these policies, such events are being reported on a regular basis. Such regular accidents imply, that all those policies and protocols are not being implemented by the healthcare workers and hence we need means of establishing the implementation of these policies. Patient-reported experience measures, are directly from the patients and hence are automatically validating the implementation of various policies and protocols.
Patient and family involvement in care has been shown to provide numerous benefits and it is imperative for the healthcare providers to ensure the same.
What are PREMs?
As per Jo Ravelingien 3 Patient patient-reported experience measures are specific self-reporting instruments that measure patients’ perception of experience while receiving care.
PREMs are basically a questionnaire-based survey that the patient is expected to take based on their perception. It is a tool that helps in assessing whether the intended actions are being performed by the healthcare workers. For example, if a question asks the patient whether all their questions related to a surgical procedure were answered to their satisfaction? An affirmative answer by all patients establishes that the surgeon is explaining the surgical intervention in detail, to all patients whereas if some patients give a negative response to the same question, it obviously implies that the surgeon needs to explain the procedure in detail to answer all the questions of patients and/or their families. This way PREMs act like constructive feedback directly from the patients and thus it is a useful measure of what happens during a care episode. It is a good tool to evaluate if the healthcare professionals are following various safety procedures and protocols.
Potential use of PREMs
PREMs can be used extensively for various purposes.
- To evaluate the implementation of patient centred care policies – PREMs being feedback directly from the patients, offer us an opportunity to evaluate the effective implementation of all patient centred care policies by the team members.
- To identify areas for improvement – PREMs can be used as a proactive measure to identify potential areas for improvement rather than waiting for an incident to happen and then reactively taking corrective actions.
- To assess the effectiveness of corrective actions – Whenever any corrective and preventive actions are implemented, the effective implementation of those actions can be evaluated using PREMs.
- To assess and improve (if needed) communication with patients and families
- To ensure that, the patient’s voice is documented and listened to provide individual care and enhance patient experience.
Implementing PREMs
Finalizing questionnaire There are two simple approaches to implementing PREMs –
1. Utilizing readymade PREMs Questionnaire – Various validated questionnaires are available either free of charge or on a payment basis or have been reported in peer-reviewed journals.
An organization can decide to opt for one of those questionnaires. The Agency for Healthcare Research and quality (AHRQ) has published various questionnaires based on the type of facility, or disease-specific questionnaires are also available on their website.
Some examples include the Accident and Emergency Department Questionnaire 4 (AEDQ), the National Inpatient Survey, the navigated transcranial magnetic stimulation (nTMS) –PREMS5, and the Consumer Assessment of Healthcare Providers and Systems (CAHPS) PREMS6, amongst others.
2. Preparing a bespoke questionnaire
- Conducting a pilot test before implementation is crucial.
- Once the questionnaire is made, assess ease of understanding to ensure optimal usage. Remove any unclear or unnecessary questions.
- Test the questionnaire in small different groups of patients. Having a multilingual questionnaire is useful in view of global medical travellers.
- Define the number of times the PREMs tool will be given to the patient. For example for a patient who is planning to undergo surgery, the first PREM questionnaire can be given after the first meeting with the surgeon and the second time during the postoperative stay.
- Various modes can be utilized like face-to-face interviews, written mail, over the telephone, or using electronic forms which comply to data security guidelines.
- Sharing forms with patients using QR codes is one cost-effective and easy way if the patient uses a smartphone.
- Asking the patient to fill the form in front of the treating clinician or staff should be avoided.
- Analyse the validity of responses and measure the time taken to complete the questionnaire.
- If any changes are made after the pilot–retesting is recommended.
- Data Collection and Measurement
- Educate patients on the purpose of PREMs and how it will benefit them.
Explaining the importance of taking the survey and differentiating it from other service feedback is essential to generate a reasonable response rate. Define the time frame of data analysis and share results with relevant stakeholders. It is advisable to refrain from taking feedback from patients who may be unable to provide precise information due to their current condition.
Limitations of PREMs
PREMs indicate a patient’s perception of the quality of healthcare, not a direct measure of patient outcome/patient’s clinical condition. Interpretation of PREMs in conjunction with data from PROMs is recommended as best practice; however, the availability of tools and challenges to capture multiple forms is practically difficult in the current scenario.
Experience in Implementing PREMs
1. Perioperative PREMs
The operating room complex is a critical area for patient safety, and in many facilities, it is heavily dependent on reporting incidents and near misses by team members.
This project looked at the complete perioperative experience of a patient and thereby helped in understanding how effectively the teams communicated with the patients. This bespoke questionnaire included questions about the patient’s experience with advice regarding preoperative fasting, clearing doubts about surgery, satisfactorily answering all questions about the type of anaesthesia, involving the patient in surgical site marking, and hand hygiene compliance of healthcare providers.
This project was conducted at two of the group hospitals from June 2021 to June 2023. A total of 5058 patients took this survey and the answers to all questions were affirmative, indicating a very robust implementation of our patient safety policies and a very clear communication by the team members.
2. PREMs on MRI safety
The MRI unit in the hospital was a busy unit as the hospital catered to huge orthopaedic load. Usually, busy units in any hospital are prone to accidents due to miscommunication, and MRI is one diagnostic facility where we need very close and clear communication with the patients. Lack of clear communication of safety precautions inside the MRI suite can lead to disastrous consequences and hence it was decided to use PREMs to assess the degree of clear communication with patients about MRI.
The bespoke questionnaire included questions such as :
- Were you advised about not carrying any metals inside the MRI scanner? (yes/no)
- Were you asked about any previous surgery that included inserting metal clips or plates? (yes/no)
- Were you asked about pregnancy?
- Were you advised about seeking help during the scan?
- Were you advised about avoiding any movement during the scan?
- Were you explained about the closed space inside the scanner?
- Were you explained about the loud noise you will hear during the MRI Scan?
- Were you offered earplugs during the scan?
- Were you offered an option of doing the scan under sedation? (yes/no/NA)
- If you were advised sedation, were you explained about fasting (yes/no/NA)
The literature search for similar PREMs questionnaire yielded no positive results, but an article published on MRI safety 7 validated the questions being asked in the questionnaire. This project has been conducted in the facility since June 2021 and so far generated 1880 responses, and none of the patients reacted negatively to any of the questions, indicating proper communication by the team members.
3. PREMs based on International Patient safety Goals (IPSG)
PREMs based on International Patient Safety Goals (IPSG) and the bespoke questionnaire include questions to evaluate whether the staff are following IPSG guidelines, such as identification of patients, maintaining proper communication, medication safety, etc.
4. PREMs based on Obstetric services
Another questionnaire developed was on obstetric services related women’s experience during delivery while at the hospital under four headings:
1. Healthcare Responsiveness
2. Pain Relief
3. Birth Experience
4. Continuity of Care
Conclusion
To summarize, PREMs offer great insights into what is happening on the ground. The chances of any intentional/ unintentional bias are minimal as it comes directly from the patients.
If appropriately implemented, PREMs can be a great proactive tool to ensure good quality of service rather than depending on near misses or incidents to happen and be reported. PREMs offer a unique opportunity to directly involve the patients in their care as they are essential stakeholders in the quality of care.
References
- W.T. Mehtsun, A.M. Ibrahim, M. Diener-West Surgical Never Events in the United States DOI: https://doi.org/10.1016/j.jvs.2013.05.040
- 81.Anna Fleck, May 2022. The NHS’s Most Serious (and Avoidable) Errors of 2021, https://www.statista.com/chart/27444/nhs-never-events/c
- Jo Ravelingien, November 2020. Everything you need to know about PROMs and PREMs, https://www.remecare.eu/blog/everything-you-need-to-know-about-proms-and-prems
- Bos N, Sizmur S, Graham C, van Stel HF. The accident and emergency department questionnaire measures patients’ experiences in the accident and emergency department. BMJ Qual Saf. 2013;22(2):139-146.
- Patel S, Ghimire P, Lavrador JP, et al. Patient-reported experience measures in patients undergoing navigated transcranial magnetic stimulation (nTMS): the introduction of nTMS-PREMs. Acta neurochirurgica. 2020;162(7):1673-1681.
- CAHPS Patient Experience Surveys and Guidance. Content last reviewed May 2022. Agency for Healthcare Research and Quality, Rockville,MD.https://www.ahrq.gov/cahps/surveys-guidance/index.html
Authors
-
-

Secretary General, CAHO, Quality Manager & Associate GS, Christian Medical College, Vellore
-

Associated Consultant Infection Diseases And HIC officer Meenakshi Mission Hospital, Madurai
-

Project Co-lead for PREMs; CAHO; Consultant Quality and Patient Safety AGM Medical Affairs and Quality ; Aster DM Healthcare, Dubai, UAE
-

Project lead for PREMs; CAHO; Medical Director & Head of Anaesthesia Medicare Orthopedics and Spine Hospital Dubai-UAE



