Experiential Learning from Multiple Accreditation Systems
Read the Magazine in PDF
Abstract
Experiential learning in healthcare is influenced by multiple accreditation systems, shifting from quality assurance to continuous quality improvement. The emphasis is on patient-centric approaches, sustainability, and digitization. Challenges like cultural diversity and clinical governance are addressed, with patient feedback and participation being central. The article compares accreditation programs, highlighting common elements and unique aspects. Patient perspectives drive excellence through accreditation.
Introduction
Accreditation focusses on established criteria and compliance to the same. A patient-centric approach has gained prominence, emphasizing quality systems aligned with patient needs. Sustainability and continual improvement analysis are vital to showcasing progress over time. Accreditation evaluations revolve around safety, equity, efficiency, timeliness, effectiveness, and patient-centeredness.
Components of the accreditation process
In any accreditation process, leaders’ active engagement is crucial. Operational efficiency, cost-effectiveness, attention to detail, and leadership involvement are sought after by organizations. A common thread among accreditations is global standardization. Effective preparation and time management are essential for success.
Embracing digitization has become vital due to its increasing importance in healthcare. A recent JCI accreditation employed innovative technology, enhancing credibility and reducing bias. While digitization may present challenges, India’s progress in this area is promising. Ultimately, the focus remains on people and continuous quality improvement, with digitization being an important consideration in the accreditation journey.
Data is a standard element, and while it is not the focus now, it’s worth noting that quality assurance is often seen as the ultimate goal of accreditation. When we examine quality assurance, it primarily involves ensuring compliance with established standards. However, a common challenge arises when organizations encounter non-compliance, and the mindset of overlooking less critical processes can weaken the overall system. This raises the question of whether quality assurance is the ultimate objective or if there is room for improvement.
The Journey of Accreditation
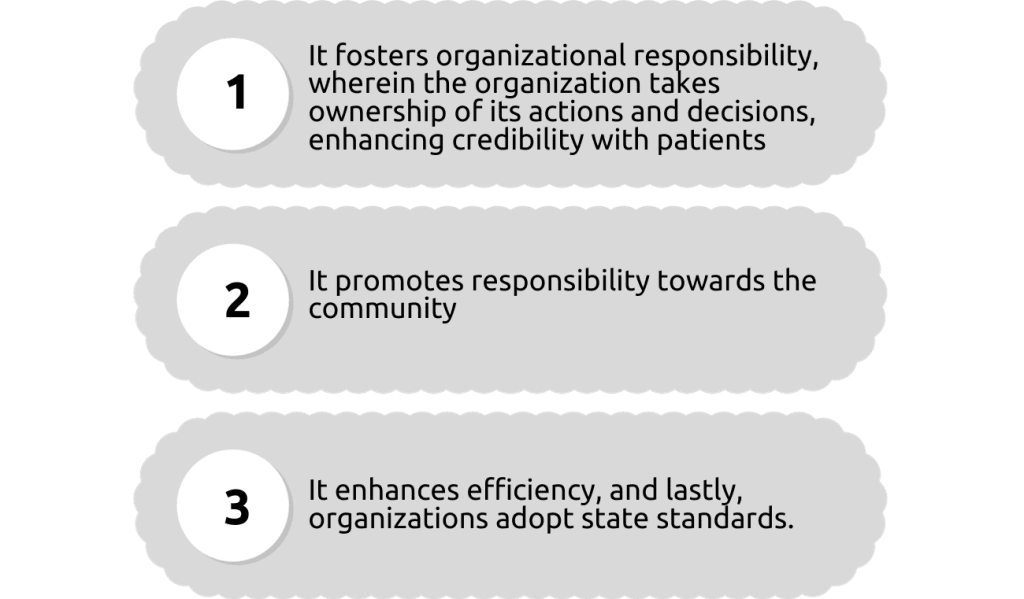
The significance of quality improvement is crucial, moving organizations from focusing on quality assurance to embracing continuous quality improvement (CQI). This non-punitive approach involves recognizing, measuring, analyzing, and monitoring areas for enhancement, ultimately leading to excellence, which is the goal sought by patients. Learning from the accreditation process yields several benefits for organizations;
Challenges like cultural diversity must be understood as they can impact standards’ application in different countries. Gender considerations may affect specific procedures. Clinical governance is another vital aspect of healthcare. The following slides will compare various elements related to accreditation.
Accreditation Programs
In the ecosystem context, each accreditation program focuses on specific aspects. One key consideration is the end-to-end process. Accreditation bodies evaluate whether the organization has a comprehensive strategy that begins when the patient arrives and continues even after they have left. The importance of this approach has been accentuated during the pandemic, where home care and post-treatment monitoring have become essential for patient safety and well-being. Thus, home care has become an integral part of the accreditation process. Sustainability is another critical aspect assessed by quality-driven accreditation programs. They examine whether the processes in place are not only repeatable but also sustainable over the long term.
Organizational satisfaction and growth, along with risk mitigation, are also taken into account, with some accreditation standards even emphasizing the establishment of a risk committee. When comparing different accreditation programs, we can find similarities and distinctions. NABH, for instance, emphasizes continuous quality improvement (CQI), while JCI emphasizes innovation and guides organizations through the surveillance process. ACHSI, on the other hand, has a unique approach that heavily prioritizes patient feedback, conducting interviews with patients and staff to ensure patient-centricity. Additionally, patient response and participatory decision-making have become crucial in the current environment.
Conclusion
The patient’s perspective is paramount in every accreditation process. Patients’ needs, safety, and feedback are central to achieving excellence and ensuring quality healthcare services. By incorporating patient-centric practices, organizations can enhance their overall performance and create a patient-centered ecosystem. Thank you for your attention.