Patient Safety: Checklists, Culture and the Patient´s Perspective
Read the Magazine in PDF
Abstract
The article discusses patient safety, interventions, and factors affecting outcomes based on Western European studies. Tailored patient safety strategies are crucial for diverse healthcare settings, especially in India with its double burden of disease. The study introduces a survey tool focusing on five domains of patient experience, emphasizing ongoing interaction between patients and healthcare professionals for quality improvement. Challenges and opportunities of involving patients in quality improvement are highlighted, including addressing cultural and structural barriers to patient-centered care. Low patient involvement in formal quality and safety roles in European hospitals calls for further discussion and action.
Introduction
This research study examines checklists, patient perspectives, and healthcare culture, with a focus on social science and public health. It analyzes disability-adjusted life years in Western Europe, highlighting the contributions of diseases. In India, a double or triple burden of disease is observed. The findings are crucial for healthcare and patient safety strategies in India, considering variations in healthcare quality across the country. The author of this study acknowledges limited familiarity with the Indian healthcare system and no conflicts of interest.
What is patient safety?
Patient safety is a comprehensive framework that aims to lower risks, prevent avoidable harm, and reduce the impact of damage in healthcare. It covers all aspects of care delivery and impacts various outcomes, both immediate and delayed [1].
Epidemiology of patient safety
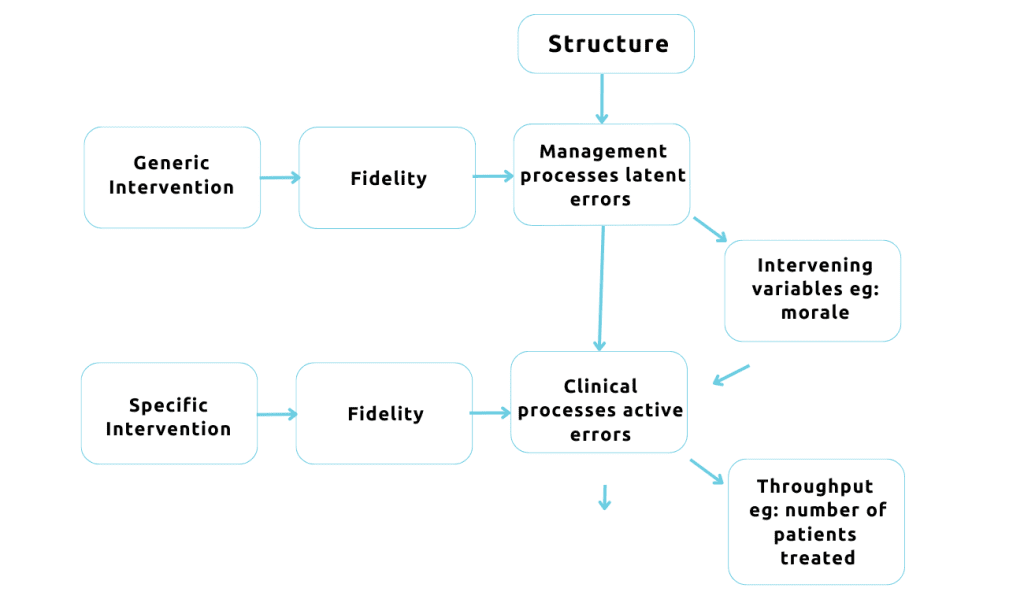
Avedis Donabedian’s structure-process-outcome model is crucial in understanding patient safety. The UK divides patient safety into components driven by healthcare professionals, management, and design processes. The image shows the need to address both structural and process factors to enhance patient safety’s complexity [2].
Any intervention to improve patient safety can first be distinguished as:
- Generic intervention
- Specific intervention
Fidelity is crucial for patient safety interventions. Factors like latent and active errors, infrastructure, and patient volume impact safety. Research methods, including retrospective reviews, identify causal factors for harm in approximately 10%
of patients [3].
The European DUQUE study investigated quality management, clinical processes, and outcomes in hospitals. External pressures, governance, and culture influence decision-making and data utilization. Organizational culture and professional engagement are essential for effective hospital-wide quality improvement. The study collected patient safety, care outcome, and perception data at the department level in European hospitals [4].
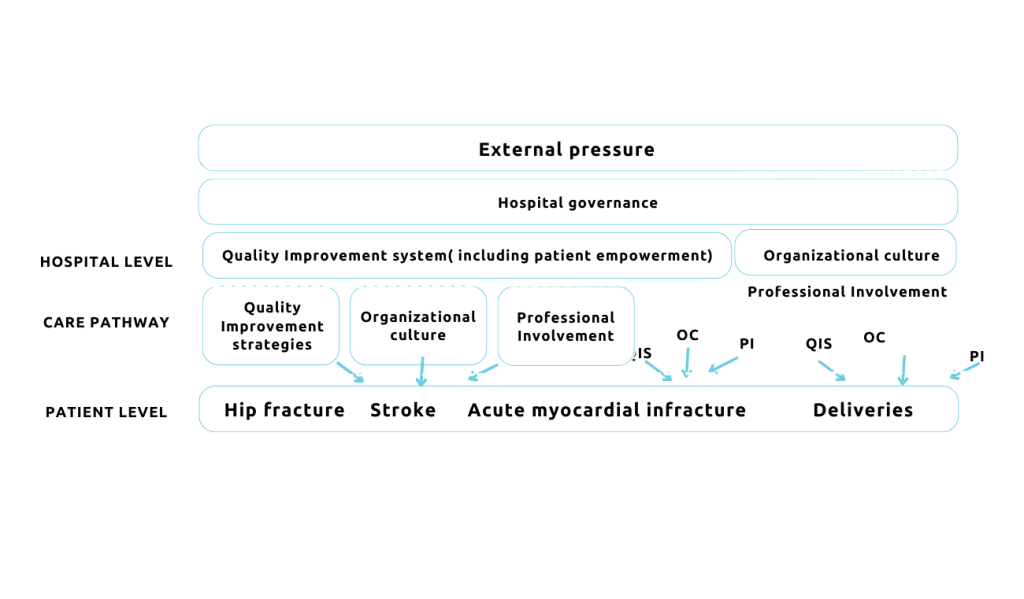
A Conceptual model for the multi-level DUQUE study: constructs and hypothesized relationships.
Patient Safety Practices
Sunol and Arah’s paper identifies evidence-based patient safety practices like pre-operative checklists and hand hygiene, widely recommended in Europe. Implementing such procedures is a topic of study, especially in Western Europe. Patient safety strategies can focus on specific areas or broader care pathway organization. The “Deepening Our Understanding of Quality Improvement in Europe” study assessed indicator implementation in 74 acute care hospitals across seven countries, identifying variations within and between nations and hospitals.
Sunol et al. examined patient safety strategies (PSS) and evidence-based organization of care pathways (EBOP) guidelines in 74 European hospitals, assessing implementation variations across countries and departments. Significant disparities between evidence and practice were found, influenced by country and within-country differences. Organizations should evaluate current implementation approaches to support PSS and EBOP effectively. Compliance with patient safety practices varied across diseases and countries, hindering comparisons. Consistent and uniform implementation is crucial to achieving optimal patient outcomes and meeting safety standards.[3]
Patient Safety Culture
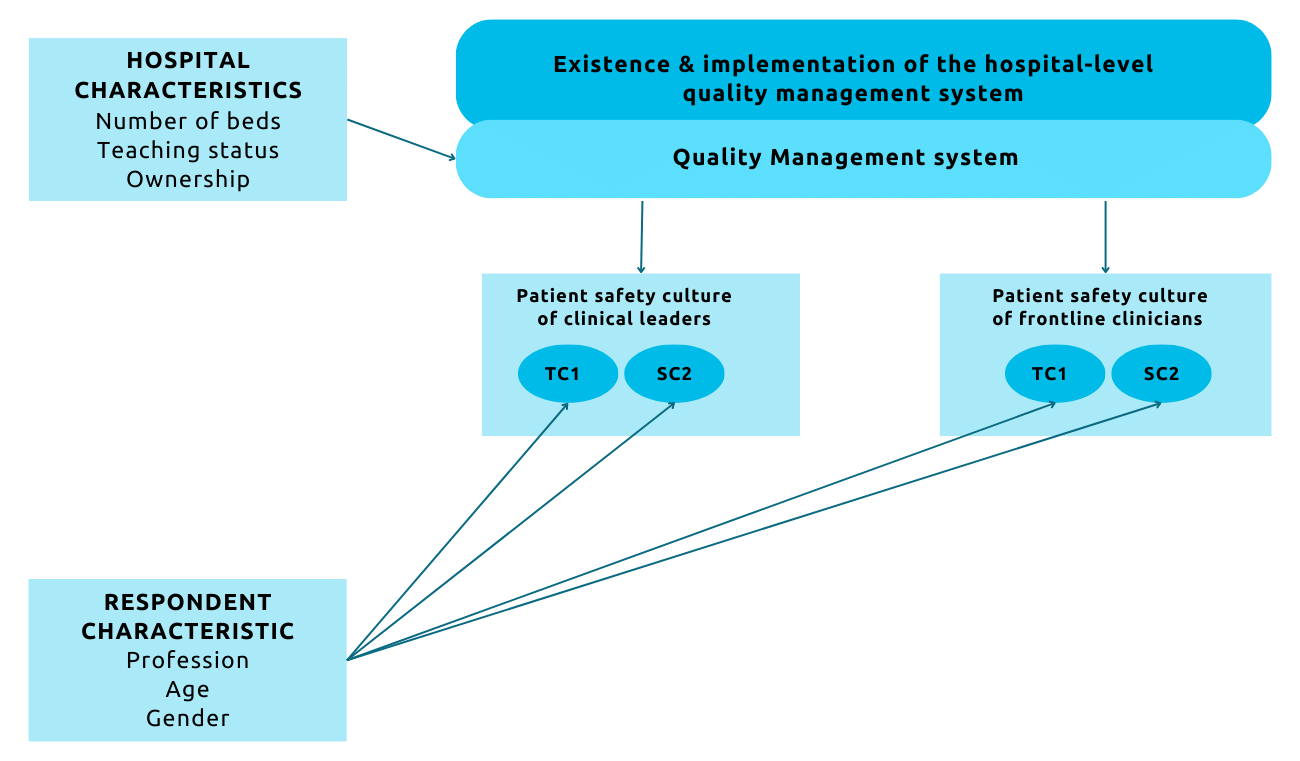
Researchers conducted a study to explore the causes of variability in hospital performance, focusing on factors like hospital type, ownership, and catchment area. They investigated the “patient safety culture” concept and its relationship with other quality management components like accreditation and standard operating procedures. Surveys in seven European countries highlighted the significance of patient safety culture in hospital performance and the importance of consistent quality management systems to support it [5].
Kristensen et al. studied the relationship between quality management systems and teamwork and safety climates in European hospitals. Positive associations were found, but perceptions differed between clinical leaders and frontline clinicians. The study highlights the importance of quality management systems in fostering a safe climate and teamwork. Further research is recommended to gain a deeper understanding, considering variations in healthcare professionals’ perceptions. [4]
The studies explored perceptions of teamwork and safety climate among clinical leaders and frontline clinicians. Clinical leaders reported a more positive teamwork climate than frontline clinicians, and there was a significant gap between physicians and nurses. These findings highlight the importance of a positive teamwork climate for patient safety, as issues in this area could lead to safety concerns. Interdisciplinary teamwork and communication are crucial for patient safety, emphasizing the need to address these disparities.
The Patient Perspective
When evaluating patient safety, some aspects may be challenging for patients to assess, like medication storage.
However, patients with chronic conditions requiring multiple medications and care from different providers can offer valuable input to evaluate patient safety.
To measure patient experience and patient safety in primary care, a concise measure was developed that focuses on five domains:
- Access to appointments
- Staff friendliness
- Consultation interactions
- Medication errors
- Care coordination
To assess patient safety, patient input is valuable, especially for those with chronic conditions and complex medication needs. Communication issues between patients and healthcare providers can lead to medication misunderstanding and adverse events.
Implementation of patient safety surveys is often inadequate, and data utilization by healthcare providers needs improvement. There is a need to work with patient-collected data to enhance patient safety evaluation.
- In a qualitative study, Bergerum et al. examined patient involvement in quality improvement in a Swedish hospital. Patients and healthcare professionals stressed the significance of organizational structure and culture. Effective communication and collaboration were deemed crucial, but barriers in complex hospital settings hindered implementation. Understanding these factors is vital for sustaining learning and change at the team level in healthcare [6].
Patient and public involvement in healthcare is gaining importance. Various initiatives in Western countries focus on engaging patients beyond just being subjects of inquiry. This broader field, known as patient and public involvement, includes terms like user involvement, patient representation, and lay involvement.
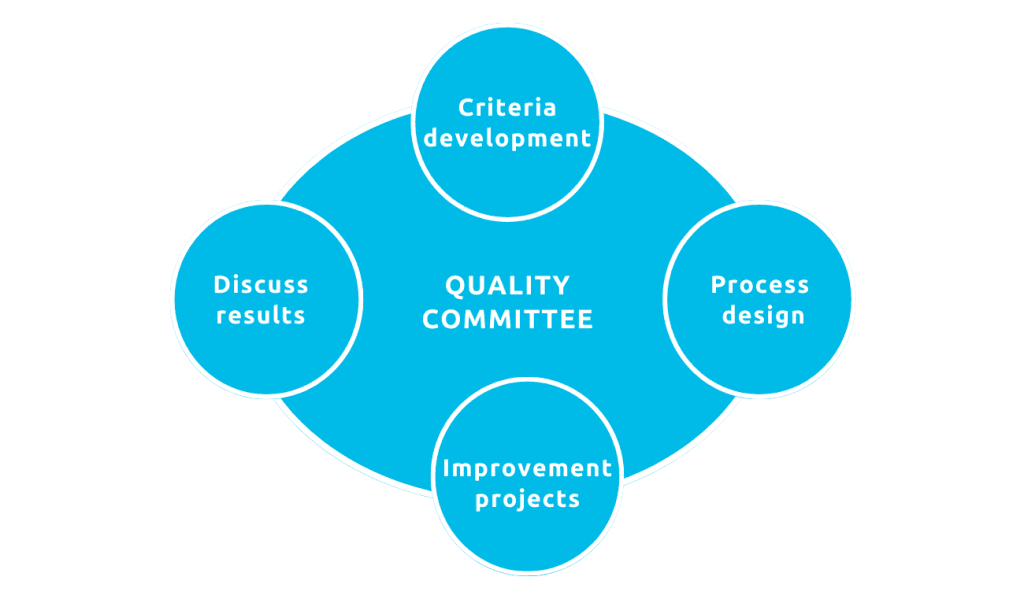
Patients can contribute to improving healthcare through their involvement in quality management planning, design, and evaluation. However, the survey results reveal that patient involvement in formal roles related to quality and patient safety in European hospitals is limited. Patients are rarely included in the development of quality criteria or the organization of care processes, despite being the ultimate beneficiaries of care. The UK shows progress in appointing a chief patient director to address patient-centered care issues, promoting patient involvement at the highest level of organizations. Adaptation of care processes and involving patients in care pathways are crucial for enhancing patient-centered care.
Towards an integrative approach
A systematic review was conducted to understand the factors contributing to high performance in hospitals. Out of 11,428 studies, 19 were analyzed, revealing seven key themes: positive organizational culture, senior management support, performance monitoring, a professional workforce, effective leadership, expertise-driven practice, and interdisciplinary teamwork. These factors were interdependent and essential for successful performance. [7]
- Taylor et al. conducted a qualitative systematic review to identify factors and strategies associated with high-performing hospitals. Seven themes emerged, including positive organizational culture and effective leadership [7].
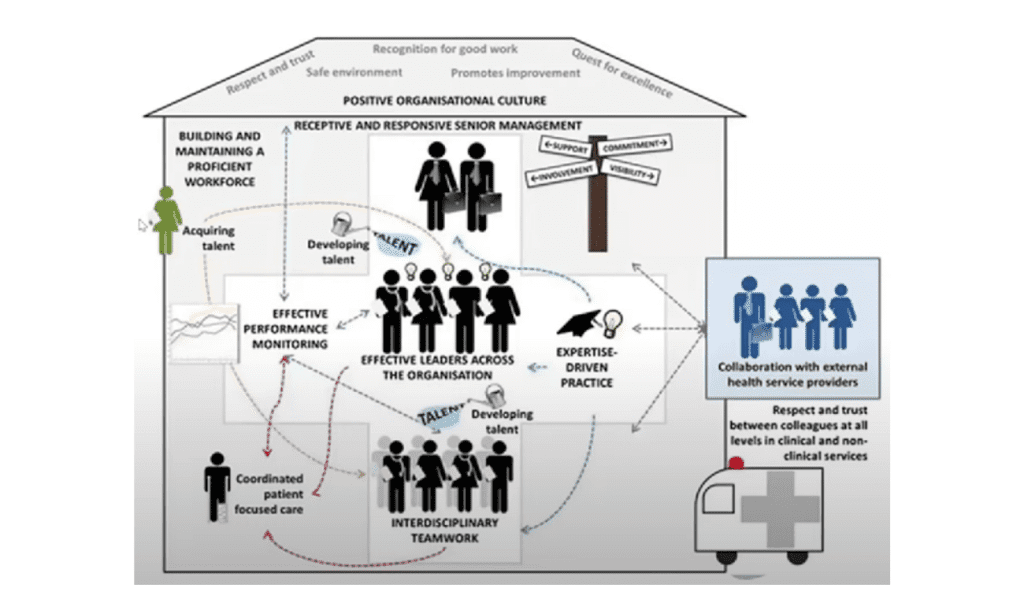
- The review identified 56 practical strategies for achieving high performance, emphasizing the need to understand and leverage these factors for ongoing improvement in hospitals.
Conclusion
The study explores patient safety, illness burden, and evidence-based practices in India and Western Europe. It emphasizes the need for a comprehensive patient safety strategy, effective governance, and patient-centered care to improve healthcare outcomes. Understanding regional differences is crucial for effective communication and collaboration in the healthcare industry. Ongoing efforts to enhance patient safety and treatment quality are vital.
References
- Groene, O. et al. (2014). International journal for quality in health care, 26(suppl_1), 2-4.
- Groene, O. (2017). Risk Factors and Epidemiology of Surgical Safety. In Surgical Patient Care: Improving Safety, Quality and Value (pp. 15-24). Cham: Springer International Publishing.
- Sunol, R., et al (2014). International journal for quality in health care, 26(suppl_1), 47-55.
- Kristensen, S., et al (2015). International journal for Quality in health care, 27(6), 499-506.
- World Health Organization. (2021). Global patient safety action plan 2021-2030: towards eliminating avoidable harm in health care. World Health Organization.
- Bergerum, C., Engström, A. K., Thor, J., & Wolmesjö, M. (2020). BMC Health Services Research, 20(1), 1-13.
- Taylor, N., et al (2015). BMC health services research, 15(1), 1-22.
Author
-

Vice Chairman of the Board, OptiMedis AG, Hamburg (Germany) Co-founder and Director Population Head of OptiMedis-COBIC UK



