Digital adaptation and clinicians Making digital DNA
Read the Magazine in PDF
The goals are to leverage technology to enhance efficiency, durability, and the results of decision-making.
and
Human empathy is an integral part of the healthcare system.
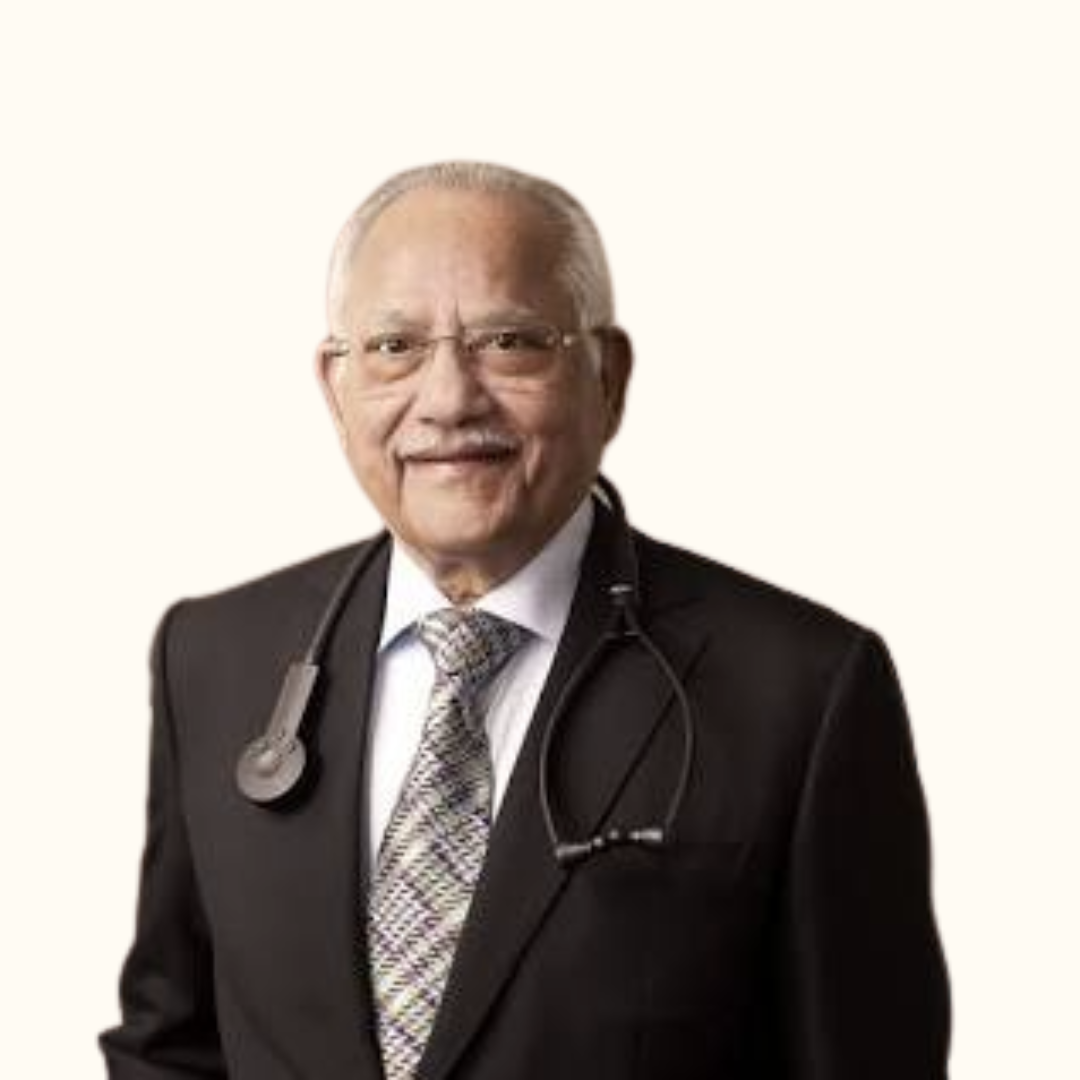
By - Dr Prathap C. Reddy & Mr Arvind Sivaramakrishnan
Abstract
The article discusses the potential of personalized care in healthcare, which requires data harmonization, insight creation, and enhanced intelligence. It emphasizes the importance of engaging clinical and ancillary participants and healthcare administrators and integrating digitalization into existing workflows to minimize disruption and ensure that healthcare providers see the benefits of electronic medical records (EMRs) firsthand. It also highlights the importance of intuitive user experience and screen design, avoiding alert fatigue, and presenting information in a structured and intuitive manner. The adoption of digital technology can be facilitated by involving all stakeholders in the conversation and creating a collaborative effort. Digitalization can help track treatment given during hospital stays and facilitate follow-up care, leading to comprehensive organizational change that enhances patient care.
Our goal is to make high-quality healthcare accessible to all people, regardless of their background. We are dedicated to achieving and sustaining excellence in education, research, and healthcare for the betterment of mankind.
Vital elements in our vision for the future are as follows:
- An unwavering dedication to clinical excellence
- A relentless pursuit of expertise
- The ever-tender Apollo empathy
- Strong focus on future-ready healthcare through education and research
“The goals are to leverage technology to enhance efficiency, durability, and the results of decision-making.”
and
“Human empathy is an integral part of the healthcare system.”
The Promise of Personalized Care
Today’s and future healthcare is focused on personalized care, which involves a combination of useful information and enhanced intelligence. Achieving this requires data harmonization and insight creation, leading to clinical decisions and actionable insights that result in improved clinical and operational outcomes. This approach answers the question “What’s in it for me?” for every individual, which is a common concern when implementing large-scale digitization and electronic medical records (EMRs). Unfortunately, many people perceive EMRs as merely an administrative burden, but this is a widespread misconception. To address people’s negative perceptions of EMRs, we must focus on the potential of personalized care. By engaging clinical and ancillary participants, as well as healthcare administrators, and emphasizing the importance of creating excellent clinical and operational outcomes through insightful data analysis, we can shift the conversation towards how to implement these systems effectively. One of the first steps in overcoming resistance is to understand why it exists in the first place. Even in cases where everyone agrees that EMRs are necessary, such as at Apollo, resistance can still occur. To address this, we need to make the implementation process as simple and streamlined as possible and integrate it seamlessly into existing workflows. By doing so, we can minimize disruption and ensure that healthcare providers see the benefits of EMRs first-hand. Incorporating digitalization into your natural workflow allows you to experience its benefits, and once users integrate it into their daily routine, it no longer feels like an added burden. Natural Language Processing (NLP) is a prime example of this, as it can convert text into discrete fields and be highly effective for doctors once parsing begins. NLP provides subjective power while also offering objective benefits at the point of care, which is crucial in India, where there is a large population in need of effective service. Post-facto analysis has limited potential, so it’s essential to integrate digitalization with operational processes such as billing and discharge procedures, which involve in-patient wait times and service aspects.
This leads to efficient utilization and shouldn’t be viewed as a standalone entity. Instead, it’s a care team cohort, with doctors, nurses, and administrative staff working together to serve patients and ensure that everyone is informed of the ongoing processes.
This exceptional coordination and harmony of operations:
- Smoothens delivery process
- Brings a sense of discipline and calmness into a difficult care process which often could be emotionally charged.
One important lesson to learn is how to make the user experience and screen design intuitive rather than intelligent. It’s crucial to remember that this is not the place to showcase engineering skills but rather to offer an interface that allows users to complete tasks easily, especially since they are likely dealing with other problems at the same time. When implementing quality guidelines such as alerts and reminders, it’s important to be mindful of alert fatigue, which can occur when too many alerts and symbols are used. If the screen is cluttered with red marks, arrows, and yield symbols, users may become overwhelmed and stop paying attention, potentially missing important information. Therefore, it’s essential to present information in a structured and intuitive manner that integrates with the natural workflow. Integrating patient pathways and clinical value is crucial, and evidence-based care practices and augmented intelligence should be considered as part of the integrated value.
Doctors are sometimes perceived as difficult, but this is not because of their inherent nature. Rather, it’s because the introduction of digital technology can disrupt their regimented, governed care process. Since they are responsible for human life, they are understandably cautious about any potential disruptions. However, when digital technology is integrated with their workflow and processes in a way that adds value, doctors are much more likely to embrace the change. The goal is not just to improve recordkeeping but to enable doctors to carry out transactions more effectively. This could involve billing, ordering supplies, documentation, care coordination, or even discussing a patient’s condition with a multi-disciplinary team.
When digitalization is seen as an enabler and a friend in the already burdened healthcare system, it can help manage change and improve operations. To successfully implement digitalization, it’s important to involve all stakeholders in the conversation, including the clinical fraternity, administrative staff, and HR personnel. This is not just an IT initiative but a core cultural initiative that requires a collaborative effort from all involved parties. By doing so, doctors and other healthcare professionals can see digital technology as a welcome change that helps them provide better care.
The adoption of digital technology in healthcare can be facilitated when doctors have access to a single health record that contains longitudinal and episodic aspects of a patient’s medical history across different areas. This allows doctors to consider a patient’s diagnosis and differential diagnosis more comprehensively.
In terms of clinical care, it’s important to look beyond just the hospital stay and consider what happens after a patient is discharged. Digitalization can help track the treatment given during the hospital stay and facilitate follow-up care. By integrating technology with a care continuum, the healthcare delivery system can effectively bring together people, processes, and technology in a constructive manner. Clinical data can now be analyzed and presented in charts to show patients the improvements in their health indicators, such as HbA1c or blood pressure. When digitalization integrates evidence-based care practices that are accepted and implemented by healthcare providers, it leads to a comprehensive organizational change that creates a movement. Digitalization is not perceived as a barrier to change management but rather as a supportive ally that facilitates effective healthcare delivery and enhances patient care.
Conclusion
Digital technology is vital for personalized healthcare and improved outcomes. To overcome resistance, involve stakeholders, integrate tech into workflows, and present info intuitively. Integration with the care continuum enhances patient care. View digitalization as a cultural initiative, not just IT, for successful implementation.